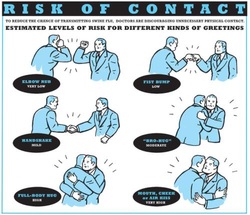
 Some studies are fascinating and disconcerting at the same time... but at least they’re good for a smile! In this paper by Ghareeb et al. the authors addressed the question whether a handshake or a fist bump is more effective in preventing or reducing pathogen transmission in the setting of a hospital, where most of us work of course. Unsurprisingly they found that using the fist bump instead of handshakes made skin contact 2.7 times shorter and this reduced spread of bacteria. They concluded that the fist bump is an effective alternative to the handshake in the hospital setting and that bumping might lead to decreased transmission of bacteria and improved health and safety of patients and health care workers alike. So shall we all start bumping around the hospital? We performed an observational study in our medium sized ICU in Galway (without approval of any committee and of course without any statistical evidence to be presented, actually just out of interest and for fun). We might also mention beforehand that working atmosphere in our unit is very good and nurses and doctors work very closely together. Interestingly, neither nursing staff nor doctors shake hands when they meet and greet each other in the ICU. The only occasions handshakes were observed are when relatives are met for a discussion or a representative of some company comes in for a visit. In regards of the study mentioned above I have some serious concerns: I wonder how many health care professionals out there would welcome a family fist bumping that has come in to discuss an end-of-life issue for instance. Also when representing the unit towards someone outside of hospital a fist bump carries some substantial risk of giving a very unprofessional impression... at least in Europe! And in very few occasions also a warm hug will be irreplaceable by some awkward bump. Social behavior is also a way on communicating... and anyhow, who pays for such studies? Ghareeb PA et al. J Hosp Infect. 2013 Dec;85(4):321-3 Picture displayed above is taken from the New York Times  JAMA just published another interesting puzzle piece on the topic of post arrest cooling. In this interesting, randomized trial, the authors addressed the question wether prehospital cooling aiming for 34°C improves outcomes after resuscitation from cardiac arrest in patients with ventricular fibrillation (VF) and non-VF. A total of 1359 patients were enrolled within 5 years. Primary outcomes were survival at hospital discharge and neurological status at discharge. In regards of primary outcomes no differences were found between the intervention and control group. Also when looking at patients who awakened from coma or died without awakening again no significant differences between the intervention and control group were found. Also length of stay, access to early coronary angiography and reduction in level or withdrawal of life support did not differ. When looking at patient safety issues though the investigators noted a higher incidence of rearrest during transport to the hospital. The intervention group (cooled out of hospital) also showed significantly lower oxygenation on arrival, increased pulmonary edema on the first chest x-ray and a greater use of diuretics during the first 12 hours after admission. During further hospitalization though the number of days ventilated, the incidence of re-intubation and the use of antibiotics did not differ. The study results don’t support the practice of out-of-hospital cooling but show some worrying implications for patients safety. Cobb LA et al. JAMA. 2013;311(1):45-52 Open access on JAMA Network Reader (Need for sign up) Recent BIJC blog on Targeted Temperature Management Trial: Targeted Temperature Management Trial: Is it Time to Stop Cooling Patients after Cardiac Arrest?  As published in the New England Journal the ALBIOS trial has already received a lot of attention and was also one of the hot topics at the ISICEM in Brussels last week. So what’s the story. First there is the original article published in the recent NEJM. Gattinoni et al. have looked into the potential advantages in giving 20% albumin and cristalloid solutions to hypoalbuminic patients with severe sepsis compared to cristalloid solutions only. In the albumin group they aimed for a serum albumin concentration of 30g/L (a number hardly ever seen in any ICU patient) until discharge from the ICU or 28 days after randomization. 1818 patients were included and to make things short: The trial found no difference in 28-day mortality (primary outcome), 90-day mortality (secondary outcome), or any other relevant clinical endpoint (number of patients with organ dysfunction, degree of dysfunction, length of stay in ICU and the hospital). So far for the original article. But now there is also this wonder-some supplementary appendix where the group has performed an unplanned subgroup analysis in septic shock patients only where a significant difference in the 90-day mortality was found - in favor for albumin. Indeed there is a lower number of deaths in the albumin group, but not in the p value when adjusted for clinically relevant variables. It might also be interesting to note that the 90-day mortality was a secondary endpoint and no subgroup analysis was performed of 28-day mortality among patients with septic shock. My personal view on this topic is that the original article and the supplemental appendix provide no good reason to favor albumin in the treatment of septic patients in general. The evidence provided to support the application of hypertonic albumin in septic shock patient is also not very convincing. In regards of the SAFE study from 2004 the use of albumin will remain controversial and it will be interesting to see further trials upcoming in this field. It is also worthwhile remembering that albumin remains reasonably expensive and as Prof. Takala, Bern Switzerland, mentioned in Brussels last week: the money saved on avoiding unnecessary albumin infusions might be better invested in other ICU resourced proven to improve patient outcome. Comments? Gattinoni L et al. N Engl J Med March 18, 2014 Gattinoni L et al. N Engl J Med March 18 2014: Supplemental Appendix SAFE study. N Engl J Med 2004; 350:2247-2256  In 2009 Haynes at al. published an article in the NEJM reporting large improvements in surgical safety when adapting the use of a standardized checklist issued by the WHO in 2008. Over the period of almost one year they looked at 8 hospitals, in 8 cities, on 7 continents. A total of 3733 patients that underwent non-cardiac surgery were enrolled to compare before and after introducing the Surgical Safety Checklist. The 2009 study found a 47% reduction in deaths associated with high-risk surgeries when the checklist was used. The rate of surgical site infections was almost cut in half and there was a significant reduction in overall complications (by 36%) and unplanned returns to theatre... Wow! The study group concluded that the checklist program has the potential to prevent large numbers of deaths and disabling complications... ‘although further study is needed to determine the precise mechanism and durability of the effect in specific settings’ And further study has been done now. Urbach et al. now has published a special article, again in the NEJM. This time they surveyed all acute care hospitals in Ontario, Canada, before and after adopting surgical safety checklists. During 3 months 101 hospitals performed 109’341 (before) and 106’370 (after) surgical procedures. In this study no significant reduction in operative mortality or complications was found... Oh! So are these checklists for no use at all or is there another explanation for these different findings? The author, Dr. Urbach, says himself that checklists are here to stay and are helpful in theatre, but that he is hopeful it will serve as a bit of a reality check to say that ‘You know it’s not this easy to create major improvements in what really is a large and complex problem’ (The Canadian Press). It also shows that checklists itself are not the only solution for problems with patients safety... especially in a time where checklists are introduced everywhere... yes, everywhere! Haynes et al. N Engl J Med 2009; 360:491-499 Urbach et al. N Engl J Med 2014; 370:1029-1038 Iodinated Radiocontrast Agents can cause Kidney Injury... But not as much as we thought they would!12/3/2014
 One major concern when bringing a critically ill patient for a CT scan is the potential for acute kidney injury (AKI) by applying iodinated contrast media intravenously. Post-contrast AKI carries the risk of more permanent renal failure, dialysis and even death. The authors of this review article nicely summarize current evidence on this issue and show, that the risk of AKI secondary to contrast material (particularly when administered intravenously for contrast-enhanced CT) has been exaggerated in the past by older, noncontrolled studies. In fact, by reviewing more recent evidence they come to the conclusion that the risk is almost nonexistent in patients with normal renal function. Even in patients with pre-existing renal insufficiency the risk of secondary contrast-induced AKI is probably much smaller than traditionally assumed. Again they emphasize on the fact that volume expansion is the only preventive strategy with a convincing evidence base. Nevertheless, the benefits of a contrast-enhanced exam still will have to be balanced with the remaining risk of AKI. BioMed Research International. 2014, Article ID 859328  The transfusion of red blood cells in the ICU remains a hot topic not only since the CRIT study and TRICC trial. It has been associated with complications and worse outcome. Unfortunately anemia and bleeding are common problems in critical care and therefore transfusions remain an important tool in the treatment in these patients, especially as we know that anemia itself is harmful. The question still remains when and in which situations RBC transfusions are indicated and helpful, especially in patients with coronary heart disease (CHD). The TRICC trial in the NEJM in 1999 concluded: ‘A restrictive strategy of red-cell transfusion is at least as effective as and possibly superior to a liberal transfusion strategy in critically ill patients, with the possible exception of patients with acute myocardial infarction and unstable angina’. The clinical practice guidelines from the AABB in 2012 noted that they can not recommend for or against a liberal or restrictive transfusion threshold for stable patients with acute coronary syndrome Now JAMA addresses the issue of transfusion in patients with CHD undergoing percutaneous intervention (PCI). In this retrospective cohort study they looked at 2’258’711 patients (now that’s a number) in 1431 hospitals who underwent PCI in a period of almost 4 years. Despite a considerable variation on blood transfusions practices among these US hospitals, the receipt of transfusion was associated with increased risk of in-hospital cardiac events (myocardial infarction, stroke and hospital death). ... another puzzle piece towards restriction? Sherwood M et al. JAMA. 2014 Feb 26;Vol 311, No.8 Look up here: The TRICC trial and the CRIT study (the ‘need to know’s) A short educational overview can be found here: http://lifeinthefastlane.com/education/ccc/blood-transfusion-in-icu/ Clinical Practice Guidelines from the AABB 2012: Ann Inten Med. 2012;157:49-58 Clinical Practice Guidelines 2009: Red blood cell transfusion in adult trauma and critical care, Crit Care Med 2009 |
Search
|


 RSS Feed
RSS Feed


