 As every child already knows by now the study by Rivers et al. in 2002 has raised the awareness about sepsis and led to the establishment of the surviving sepsis campaign. As we have posted on BIJC before, many elements of the early goal directed therapy (EGDT) have been discussed controversially since. In order to answer some of the questions of sepsis treatment three big trials have been started, involving different parts of this world. These efforts have led to a unique situation as we now have three high quality trials looking at the classical EGDT versus 'usual care'. ARISE and ProCESS had been published before (read here) and both of them showed no difference between EGDT and 'usual care'. ProMISe included 1251 patients with severe sepsis or septic shock that were admitted to a total 56 hospitals in the UK. Again classical EGDT with measurement of continuous central venous oxygenation was compared to so called 'usual treatment'. It's remarkable to notice that in the 'usual treatment' group about half of the patient didn't get a central line and central venous oxygenation wasn't even measured in the ones who got one. And here's the result: There was no difference in 90-day mortality and no differences in secondary outcomes. In contrast EGDT actually increased costs. It has become difficult to ignore these three trials! Our conclusion: The classical EGDT therapy has ended here and now... but EGDT will keep its central role in the treatment of septic patients! Early: - Identify septic patient quickly, start screening for patients if indicated - Administer antibiotics within the first our of recognition of sepsis - Start IV-fluid therapy immediately - Take (blood) cultures as quick as possible, but do not delay antibiotic treatment Goal Directed: - Aim for a reasonable mean arterial pressure (e.g. 65mmHg) - Aim for a sufficient urinary output (0.5ml/h) - Central venous pressure (CVP) certainly and most probably central venous oxygenation (ScvO2) are not parameters to measure fluid responsiveness - Lactate remains an issue of debate Therapy: - Simple: Whatever the physician feels is best! ProMISe Trial, Mouncey et al. N Engl J Med. 2015 Mar 17. BIJC Review on ARISE and ProCESS Picture displayed taken from the Ice Cream Trilogy by Wright, Pegg and Frost Doctors Should Position their Name Tag on the Right Side of their Chest... It's Evidence Based!23/3/2015
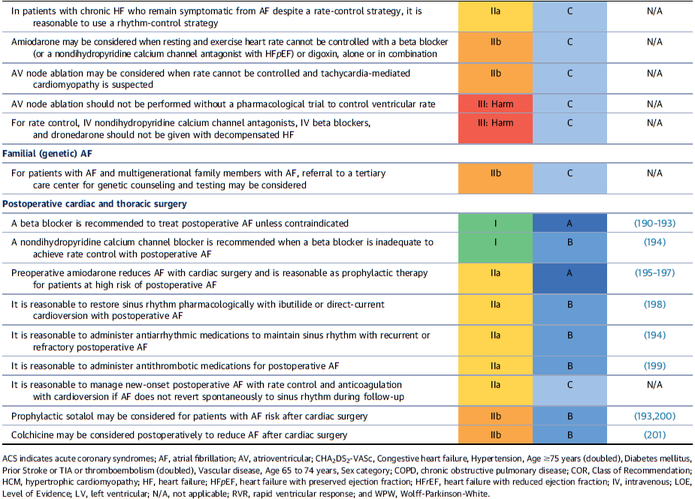
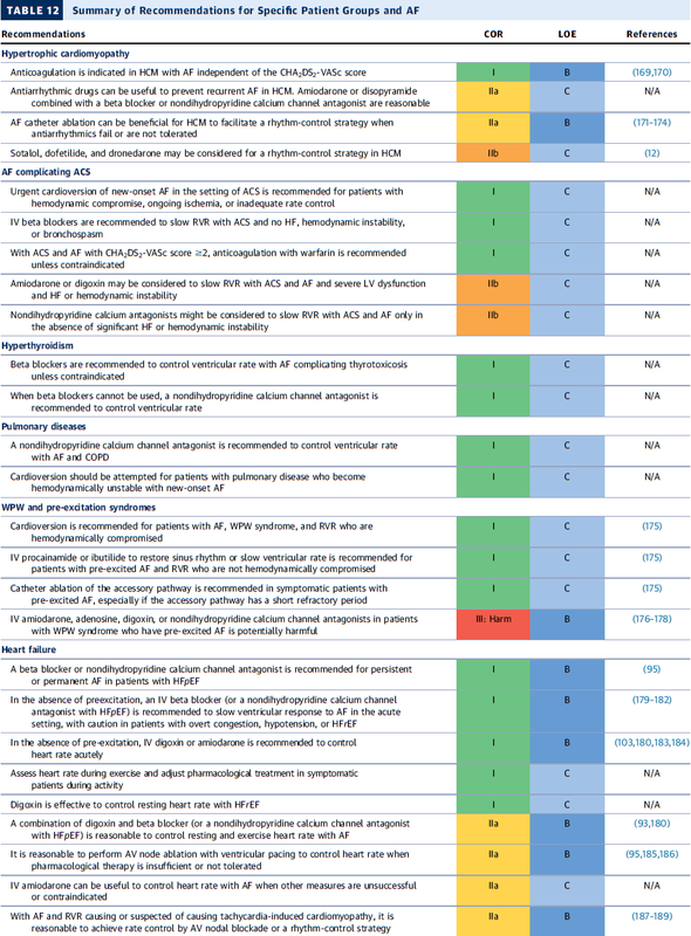
 They're All WRONG!!! They're All WRONG!!! Here it is finally, the study we all have been waiting for. 'THE question' that has never been answered... until now! Every day we all do our best to establish the best patient-physician relation possible. The first impression counts and besides introducing ourselves verbally we ware name tags to visually inform about our name and position. But did anyone actually ever ask himself if it makes a difference wether you ware your name tag on the left or right side of your chest? Well, an orthopaedic surgeon in Switzerland obviously has and conducted a 'blinded' study to answer this specific question. He made one hundred volunteers, blinded to the experimental setup, present for an orthopedic consultation in a standardized manner. The name tag of the physician was randomly positioned on the left chest side and presented to 50 individuals (age 35 years (range 17 to 83)) or the right chest side and then presented to 50 other individuals (35 years (range 16 to 59)). The time of the participant noticing the name tag was documented. Subsequently, the participant was questioned concerning the relevance of a name tag and verbal self-introduction of the physician. 38% of the participants noticed the nametag on the right as opposed to 20% who noticed it if placed on the left upper chest... hey, this turned out to be statistically significant, giving us a p-value of 0.0473! The author concludes: Positioning the name tag on the right chest side results in better and faster visibility. We conclude: - Also orthopaedic surgeons seem to be interested in a close patient-physician relationship - Orthopedic surgeons actually do talk to their patients! - Orthopedic surgeons in Switzerland don't seem to be overstrained with their workload Schmid SL et al. March 2015, PLOS One, DOI: 10.1371/journal.pone.0119042  In December 2014 the AHA, ACC and HRA have released a new bunch of guidelines on the management of patients with atrial fibrillation (AFib). The paper itself is worth reading as it looks into the basic understanding of this condition, its clinical evaluation and finally the treatment options. As these guidelines are open access it can be considered mandatory Free Open Access Meducation FOAMed. Below is a summary of the Recommendations according to specific patient groups. It's interesting to notice that digoxin still plays a role in patients with heart failure, especially when looking at the findings of Turakhia et al. in JACC, Aug 19 2014. J Am Coll Cardiol. 2014;64(21):2246-2280 OPEN ACCESS BIJC post on dixogin in critical care  Developed in the early 70'ies tramadol has become a very popular drug for pain relief for various reasons. Among others it is often said that tramadol is safe to use and has non-addictive properties, making this an ideal opioid to use for in and out of hospital. The facts though point in the opposite direction. In JAMA Internal Medicine Fournier et al. have just published a case control analysis to look at the fact that tramadol before has been associated with the occurrence of significant hypoglycemia. Their cohort included a total of 334'034 patients whereas each case of hospitalization for hypoglycemia was matched with up to 10 controls on age, sex, and duration of follow-up. Basically they compared similar patients which were either started on tramadol or codeine for pain treatment. They were able to show that compared with codeine, tramadol use was associated with an increased risk of hospitalization for hypoglycemia, particularly in the first 30 days of use. It has to be noted though, that the overall incidence is low with 7 per 10'000 per annum. In the same issue's commentary Nelson and Juurlink take the opportunity to point out some other remarkable problems associated with Tramadol, again showing us that things are not a simple as we think they are. - Tramadol itself has only a low affinity to opioid receptors and mainly works over one of its metabolites: O-Desmethyltramadol (M1), which then binds to µ opioid receptors - The expression of the enzyme that metabolites tramadol to M1 is extremely variable, thus: giving a certain dose of tramadol leaves you with an unknown dose of acting opioid! - Despite suggestions to the contrary, tramadol does pose a risk for addiction - And there are increasing reports of deaths involving this drug - Other documented adverse effects are: serotonin syndrome and seizures Conclusion: Tramadol remains a non-ideal drug in the setting of an ICU. Fournier et al. JAMA Intern Med. 2015;175(2):186-193. Nelson and Juurlink JAMA Intern Med. 2015;175(2):194-195.  Microbiologically confirmed ventilator-associated pneumonia (VAP) or ventilator-associated conditions (VAC, e.g. worsening oxygenation) in intubated patients remains a major concern in ICU's. VAP is defined as a hospital-acquired pneumonia which develops within 48-72 hours after endotracheal intubation. To prevent this complication ICU's uniformly have adapted the VAP-bundle, a bunch of measures aiming to prevent ventilator-associated pneumonia. Unfortunately the evidence of the VAP-bundle is not as robust as one might think it is. Here's the evidence of some elements of the VAP bundle: - Elevation of the head to bed 45° (low evidence) - Daily sedation interruptions (the impact on reducing VAP has not been shown so far) - Daily oral chlorhexidine rinses (low evidence) ... it's most likely the combination of measures that is of benefit to the patient... hopefully! But hold on, there is another intervention that finally brings quite some evidence with it! Active suctioning of the subglottic area, where nasal-oral secretions gather and create a rich culture medium for all sorts of micro-organisms, also aims to reduce the incidence of VAP. In contrast to the classical VAP-bundle the evidence here is strongly in favour for these devices! In 2005 four registrars in cardiothoracic surgery looked into this topic and summarised their efforts online on Best Evidence Topics, best bets.org. In this blog they review 13 relevant articles on the use of subglottic suctioning and conclude: subglottic suction significantly reduces the incidence of VAP in high risk patients - which means a NNT of 8 if ventilated for more than 3 days. They also mention that this measure is cost effective, despite the more expensive tubes. In the same year Dezfulian et al. presented a systematic meta-analysis of randomized trials in the American Journal of Medicine. They ended up with 5 studies including 869 patients. They also came to the conclusion that subglottic secretion drainage is effective in preventing VAP in patients expected to be ventilated for more than 72 hours. In 2011 Hallais et al. looked into the issue of cost-effectiveness with a cost-benefit analysis. Even when assuming the most pessimistic scenario of VAP incidence and costs the replacement of conventional ventilation with continuous subglottic suctioning would still be cost-effective. In 2011 Muscedere et al. published an 'official' review article in Critical Care Medicine and also ended up with 13 randomised clinical trial, most of them the same 'BestBETs' had already identified 6 years before. It is therefore not surprising to see that they also found a highly significant reduction in VAP. They were also able to demonstrate a reduction in ICU length of stay and duration of mechanical ventilation, although the strength of this association was weakened by heterogeneity of study results. We finally would like to mention the latest randomised controlled trial on this topic which was published in Critical Care Medicine this January 2015. Damas et al. randomly assigned 352 patients to either receive subglottic suctioning or not. Again sublottic suctioning significantly reduced VAP prevalence and therefore also antibiotic use. At least we have identified one area in critical care where an impressive pile of evidence supporting the use of subglottic suctioning in long-term intubated patients is present... and even better: cost-effective analyses also come out in great favour for this measure! Take-home message: Subglottic suctioning does prevent VAP in patients likely to be ventilated more than (48-) 72 hours and should be used in these situations. Review BestBETs 2005 Dezfulian C et al. Am J Med. 2005 Jan;118(1):11-8 Hallais C. et al. Infect Control Hosp Epidemiol. 2011 Feb;32(2):131-5 Muscedere J et al. Crit Care Med. 2011 Vol. 39, No. 8 Damas P et al. Crit Care Med. 2015 Jan;43(1):22-30 |
Search
|


 RSS Feed
RSS Feed


