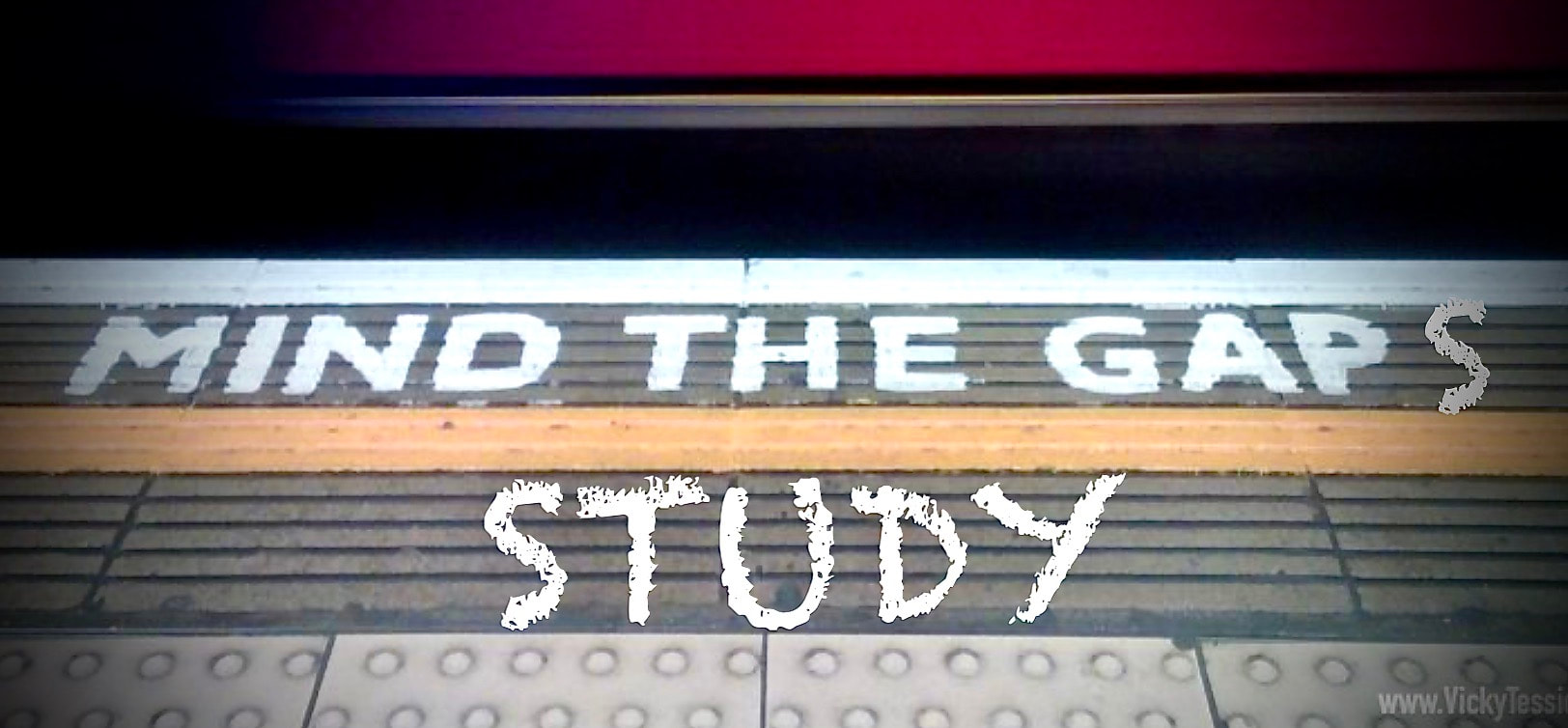
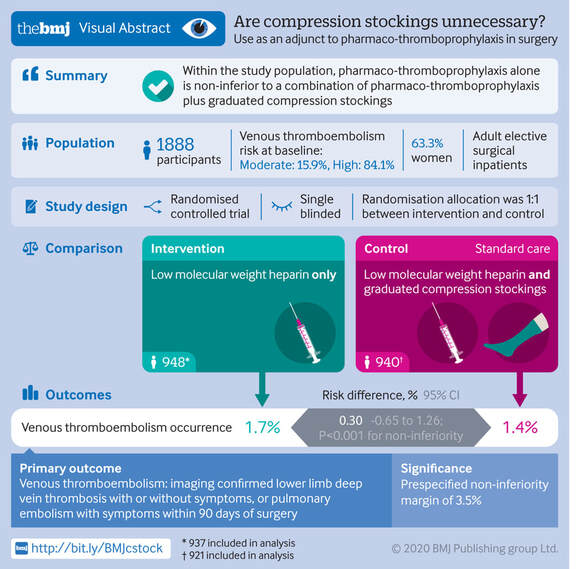
Mind the GAPS Study - Compression Stockings are Useless for Most Elective Surgery Patients!14/9/2020
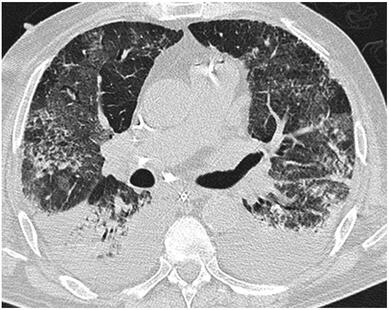
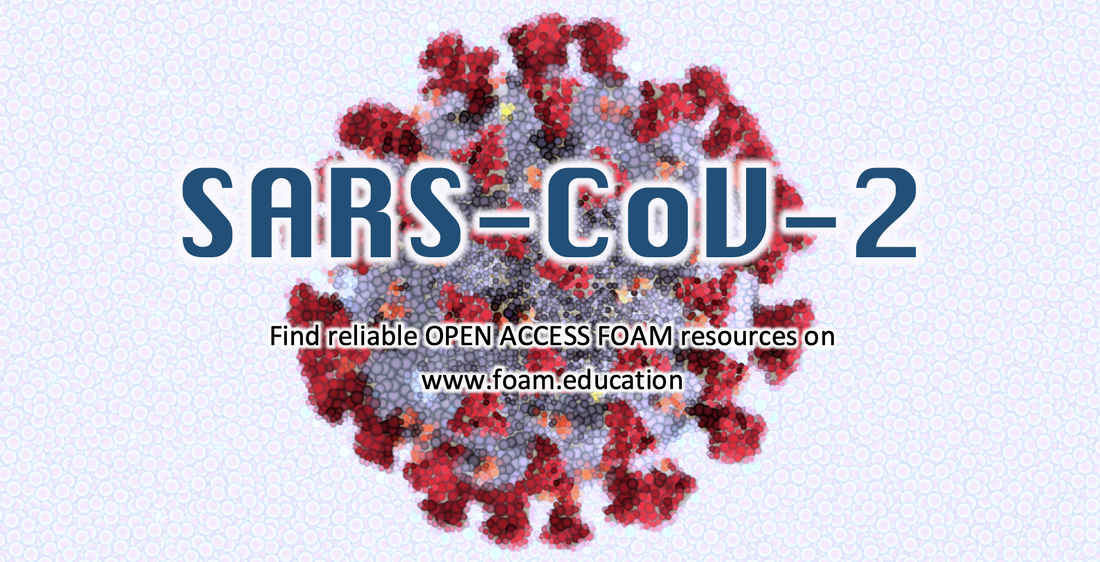
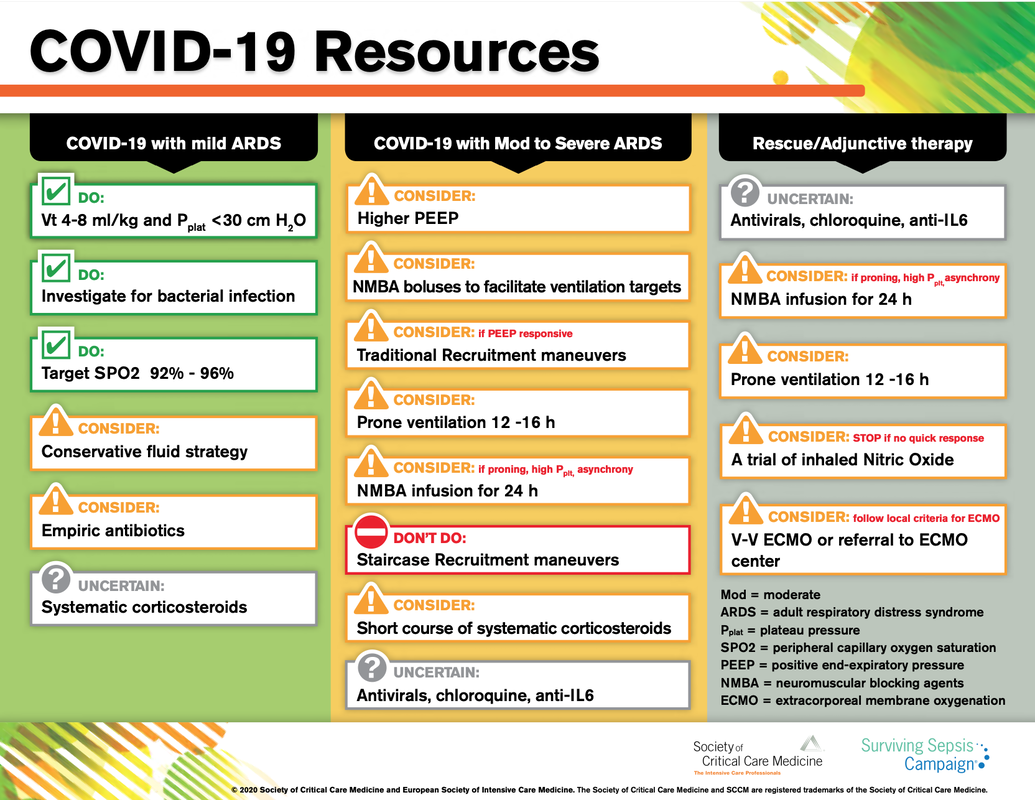
Cricoid pressure prevents aspirations, preoperative antibiotics avoid infections, and compression stockings protect against deep vein thrombosis. Many medical measures aim to reduce morbidity and mortality among patients, but unfortunately, the benefit of these measures is often not, or insufficiently, proven. Under certain circumstances, they may lead to additional problems or even cause harm (e.g. cricoid pressure Read Here). Time has definitely come to take a closer look at compression stockings for surgical patients. Apart from the fact that they look terrible, they are just as uncomfortable to wear and even carry certain risks in patients with peripheral vascular disease, for example. The effectiveness of compression stockings in modern practice has been questioned, but robust evidence has been lacking. This seems to change, as the long-awaited GAPS-Trial has been published and now provides further evidence on what concern patients undergoing elective surgery. Among this population, adding compression stockings to pharmaco-thromboprophylaxis was non-superior compared to pharmaco-thromboprophylaxis alone (primary outcome). There was also no difference in the quality of life outcomes found (secondary outcome). There is now some robust evidence to omit compression stockings in surgical patients that receive pharmacological thromboprophylaxis. Shalhou J. et al. BMJ 2020;369:m1309 The lastest updated surviving sepsis guidelines for COVID-19 patient recommends a high-peep strategy in the intubated, mechanically ventilated patient. As most of these patients present with moderate to severe ARDS, PEEP is used to keep lung areas open and therefor to improve oxygenation. This seems to be especially true in the classical case of ARDS, where the lung become 'wet' and 'heavy' which results in widespread atelectasis of the dependent parts of the lungs, often further complicated by pleural effusions. Classical CT appearance in the acute phase of ARDS is an opacification with an antero-posterior density gradient. Dense consolidation in the most dependent regions merges into a background of widespread ground-glass attenuation and the normal or hyperexpanded lung in the non-dependent areas (Howling SJ et al. Clin Radiol 1998;53(2):105-109). The theory behind these changes is that the increased weight of overlying lung causes compression-atelectasis posteriorly. The fact that prone positioning these patients quickly redistributes these gradients supports this theory (Desai SR et al. Anaesthesiology 1991;74(1):15-23). Chest CT's in patients with COVID-19 often show ground-glass opacification with or without consolidations. These are changes often seen in viral pneumonia. Several case series suggest, that CT abnormalities seem to be mostly bilateral and tend to have a peripheral distribution, often involving the lower lobes. In contrast to the classical ARDS pleural thickening, pleural effusion and lymphadenopathy seem to be a less common finding (Shi H et al. Lancet Infect Dis 2020). The leading problem in COVID-19 patients with ARDS is hypoxemia, while hypercapnia does not seem to be a significant problem. Sometimes profound hypoxemia does not seem to correlate with patient symptoms at all. In regards to the images above, atelectasis might not be the predominant reason for V/Q mismatches in these patients. Observations of mechanically ventilated patients in our unit and other hospitals in Switzerland have shown, that higher PEEP levels (15cmH2O and higher) often result in significantly reduced compliance values complicating ventilation and favouring the development of pulmonary over-inflation. This observation might support the theory that patients with COVID do not represent the traditional manner of ARDS with distinctive atelectasis. Another observation that supports this theory is that COVID-19 patients often do not respond as clearly to Prone Positioning as classical ARDS patients do. More probably, V/Q mismatch seems so happen on a more microscopical level in COVID-Patients. Lung compliance is often normal on these patients and, therefore, applying high PEEP-levels does NOT add any benefit at all. Maybe the principle of less is more also applies to COVID-19 patients we treat (Gattinoni L et al. Intensive Care Medicine; 46, pages780–782(2020)) Looking at the New Surviving Sepsis Campain COVID-19 Guidelines: Given these considerations, the strategy with High PEEP-levels in general should be questioned in principle. The European Society of Intensive Care Medicine ESICM and the Society of Critical Care Medicine SCCM have been very efficient in providing us health care workers with a guideline manuscript giving recommendations on the treatment of COVID-19 patients in a critical care setting. It is imperative to keep in mind that research is moving forward very quickly in these times and changes to these recommendations are likely to occur. A collection of many reliable OPEN ACCESS platforms on SARS-CoV-2 can be found on www.foam.education. Infection ControlWhen performing aerosol-generating procedures on patients with COVID-19 in the ICU, fitted respirator masks (N95 respirators, FFP2) should be used (in combination with full Personal Protective Equipement PPE) Aerosol-generating procedures on ICU patients with COVID-19 should be performed in a negative pressure room During usual care for non-ventilated and non-aerosol-generating procedures on mechanically ventilated (closed circuit) patients surgical masks are adequate For endotracheal intubation video-guided laryngoscopy should be used, if available In intubated and mechanically ventilated patients, endotracheal aspirates should be used for diagnostic testing Supportive CareIn COVID-19 patients with shock, dynamic parameters like skin temperature, capillary refilling time, and/or serum lactate measurement should be used in order to assess fluid responsiveness For the acute resuscitation of adults with COVID-19, a conservative over a liberal fluid strategy is recommended For the acute resuscitation of adults cristalloids should be used - avoid colloids! Buffered/balanced crystalloids should be used over unbalanced crystalloids Do NOT use hydroxyethyl starches! Do NOT use gelatins! Do NOT use dextrans! Avoid the routine use of albumin for initial resuscitation! In shock use norepinephrine/ noradrenaline as the first-line vasoactive agent The use of dopamine is NOT recommended Add vasopressin, if target MAP cannot be reached Titrate vasoactive agents to target a MAP of 60-65 mmHg, rather than higher MAP targets For patients in shock and with evidence of cardiac dysfunction and persistent hypoperfusion despite fluid resuscitation and norepinephrine, adding dobutamine should be used For persistent shock despite all these measures, low-dose corticosteroids should be tried Ventilatory SupportKeep peripheral saturation SpO2 above 90% with supplemental oxygen
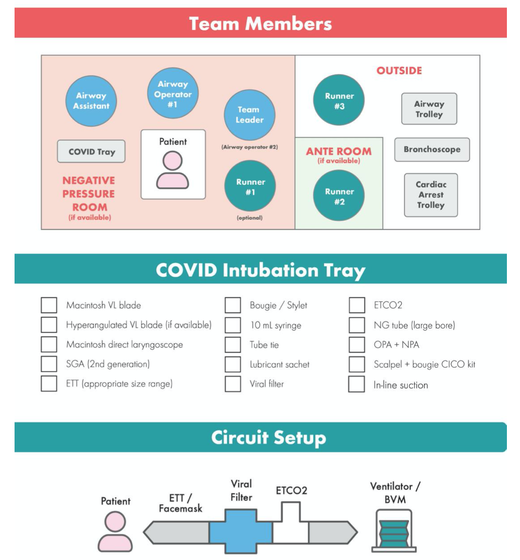
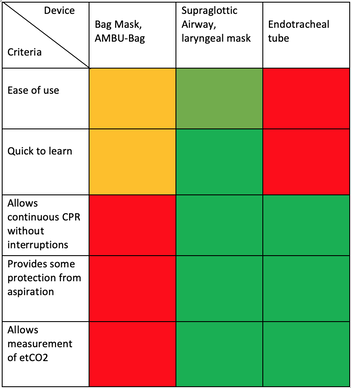
There is NO need for supplemental oxygen with SpO2 above 96% In acute hypoxemic respiratory failure despite conventional oxygen therapy, high-flow nasal cannulas (HFNC or High-Flow) should be used next High-Flow should be used over non-invasive ventilation (NIV) If High-Flow is not available and there is no urgent need for endotracheal intubation, NIV with close monitoring can be tried In the event of worsening respiratory status, early endotracheal intubation should be performed In mechanically ventilated patients, low-tidal volume ventilation should be used: 4 to 8 ml/kg In mechanically ventilated patients with ARDS targeting plateau pressures (Pplat) of < 30 cm H2O should be aimed for In patients with moderate to severe ARDS, a high-PEEP strategy should be used (PEEP >10cmH2O). Patients have to be monitored for potential barotrauma NOTE by Crit.Cloud: The strategy for high PEEP levels in general is currently discussed controversially. Observations in our own unit showed, that high PEEP levels tend to impaire compliance and therefor the quality of ventilation. Read also: "Less is More" in mechanical ventilatio, Gattinoni L. et al. Intensive Care Med (2020) 46:780-782 Patients with ARDS should receive a conservative/restrictive fluid strategy In moderate to severe ARDS, prone positioning for 12-16 hours is recommended To facilitate lung protective ventilation in moderate to severe ARDS, intermittent boluses of neuromuscular blocking agents (NMBA) should be used first In the event of persistent ventilator dyssynchrony, the need for ongoing deep sedation, prone ventilation, or persistently high plateau pressures, a continuous NMBA infusion for up to 48 hours should be used next Do NOT use inhaled nitric oxide in COVID-19 patients with ARDS routinely In severe ARDS and hypoxemia despite optimising ventilation and other rescue strategies, a trial of inhaled pulmonary vasodilator as a rescue therapy can be considered; if no rapid improvement in oxygenation is observed, the treatment should be tapered off If hypoxemia persists despite optimising ventilation, recruitment manoeuvres should be applied If recruitment manoeuvres are used, DO NOT use staircase (incremental PEEP) recruitment manoeuvres If all these measures fail, the patient should be considered for venovenous ECMO COVID-19 TherapyIn mechanically ventilated patients WITHOUT ARDS, systemic corticosteroids should NOT be used routinely In contrast, mechanically ventilated patients WITH ARDS, the use of systemic corticosteroids is recommended Mechanically ventilated patients with respiratory failure should be treated with empiric antimicrobials/antibacterial agents Critically ill patients with fever should be treated with paracetamol (acetominophen) for temperature control In critically ill patients standard intravenous immunoglobulins (IVIG) should NOT be used routinely Also, the routine use of convalescent plasma is NOT recommended The routine use of lopinavir/ritonavir (Kaletra®) is NOT recommended Currently, there is insufficient evidence to issue a recommendation on the use of other antiviral agents in critically ill adults with COVID-19 Currently, there is insufficient evidence to issue a recommendation on the use of recombinant interferons (rIFNs); chloroquine or hydroxychloroquine; tocilizumab (humanised immunoglobulin) The Aerosol-Danger of SARS-Cov-2The outbreak of the SARS Coronavirus-2 (SARS-CoV-2) in China 2019 has within a short time spread around the globe and is just about to hit central Europe. Although about 80% of all confirmed cases develop a mild febrile illness, around 17% develop severe Corona viral disease (COVID-19) with findings of acute respiratory distress syndrome (ARDS), of which about 4% will require mechanical ventilation. Since this virus, which was previously unknown to humans, spread rapidly around the globe, a large number of patients requiring intensive medical care now arise within a very short time. The lungs are the organs most affected by COVID-19 because the virus accesses host cells via the enzyme ACE2, which is most abundant in type II alveolar cells of the lungs. This results in mainly type 1 respiratory failure, which often requires urgent tracheal intubation and mechanical ventilation. Due to viral shedding in the patient's lungs, COVID-19 spread mainly via droplets. Events like coughing, high flow nasal oxygen (High-Flow), intubation and more can cause aerosol generation, allowing these airborne particles to travel even further distances. Performing endotracheal intubation in these patients is, therefore, a high-risk procedure, and it is required to adhere to certain principles to avoid infection of health care providers. The Safe Airway Societies of Australia and New Zealand have published a consensus statement that describes the problem very well and provides practical tips based on the currently available evidence. 1. Non Invasive Ventilation (NIV) and High Flow Nasal Oxygen (High-Flow)Current evidence suggests that the failure rate of NIV in COVID-19 patients seems to be similarly high as observed among Influenza A patients. Failure in these patients resulted in higher mortality. In general, NIV is recommended to be avoided or at least used very cautiously! The utility of High-Flow in viral pandemics in unknown. There is some evidence suggesting a decreased need for tracheal intubation compared to conventional oxygen therapy. High Flow Nasal Oxygen is worth a try, although it has to be assumed, that this is aerosol-generating. High-Flow should only be used in (negative pressure) airborne isolation rooms, and staff should wear full personal protective equipment (PPE) including N95/P2 masks. NIV and High-Flow are NOT recommended for patients with severe respiratory failure or when it seems clear that invasive ventilation is inevitable!
|
|||||||||||||
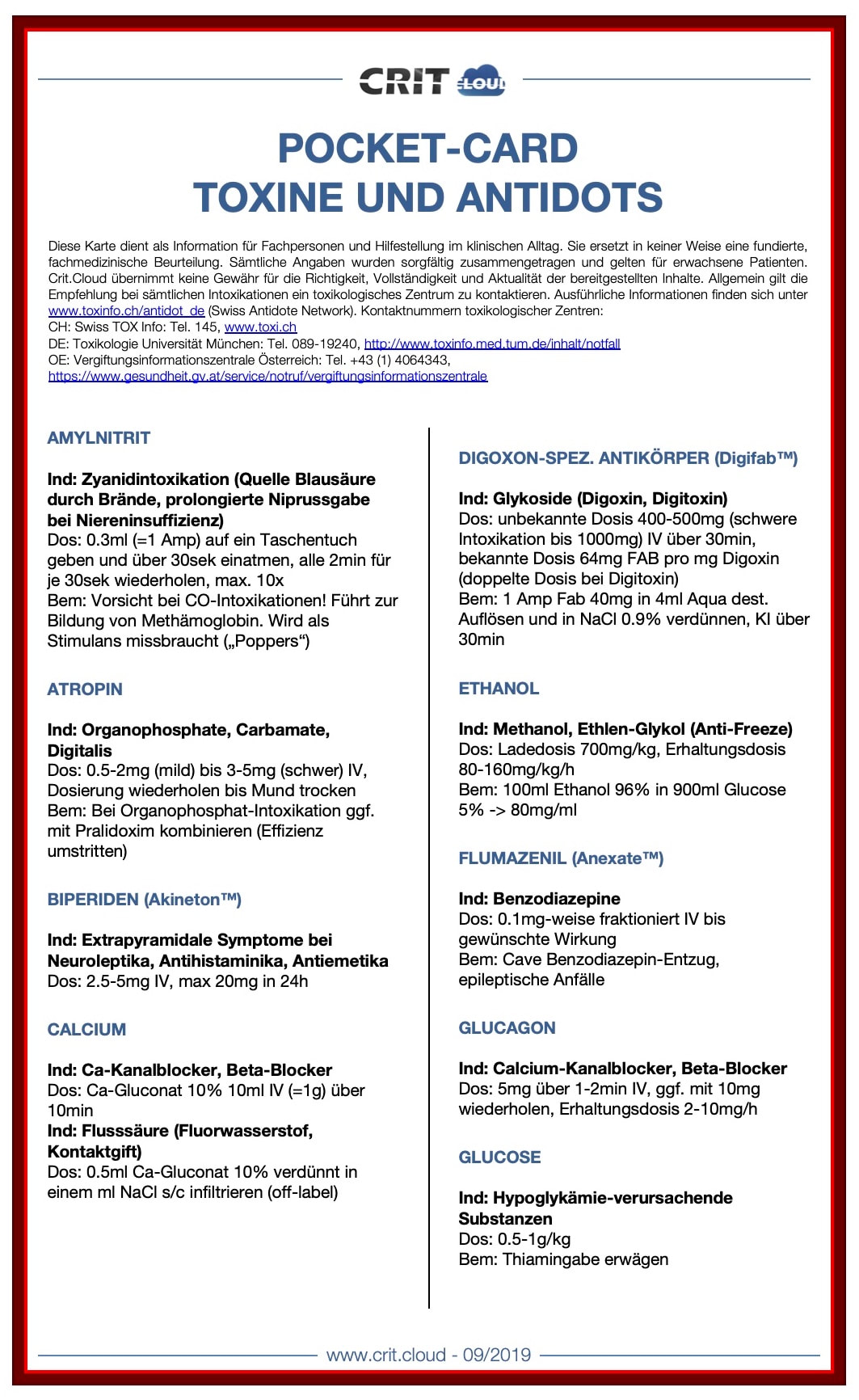
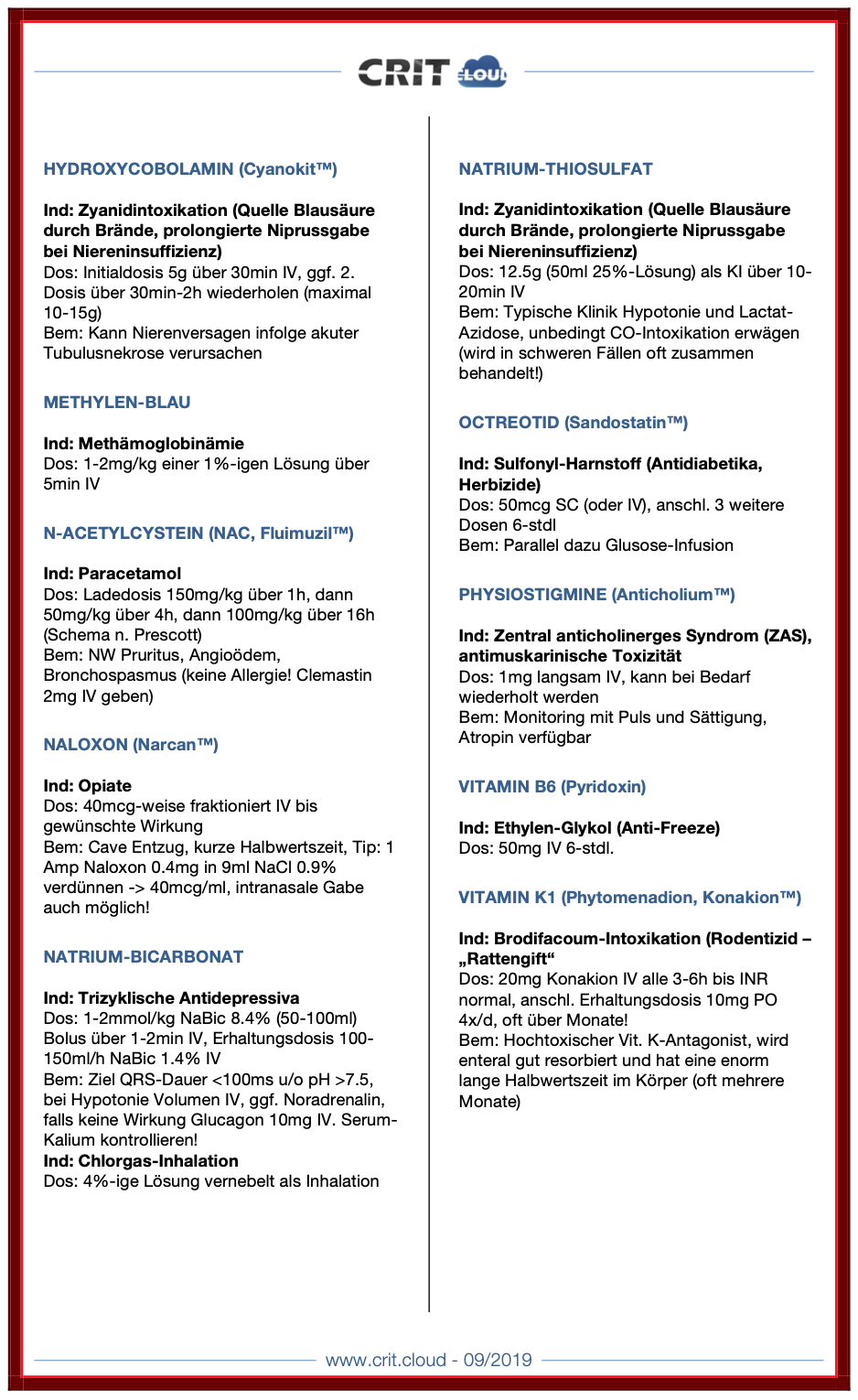
| Pocket Cards Toxine und Antidots | |
| File Size: | 165 kb |
| File Type: | |

So if you work in an emergency room, anaesthesia or intensive care, there's a good chance you will be facing an anticoagulant patient with potentially critical bleeding that could require urgent treatment... And this leaves you with the following questions:
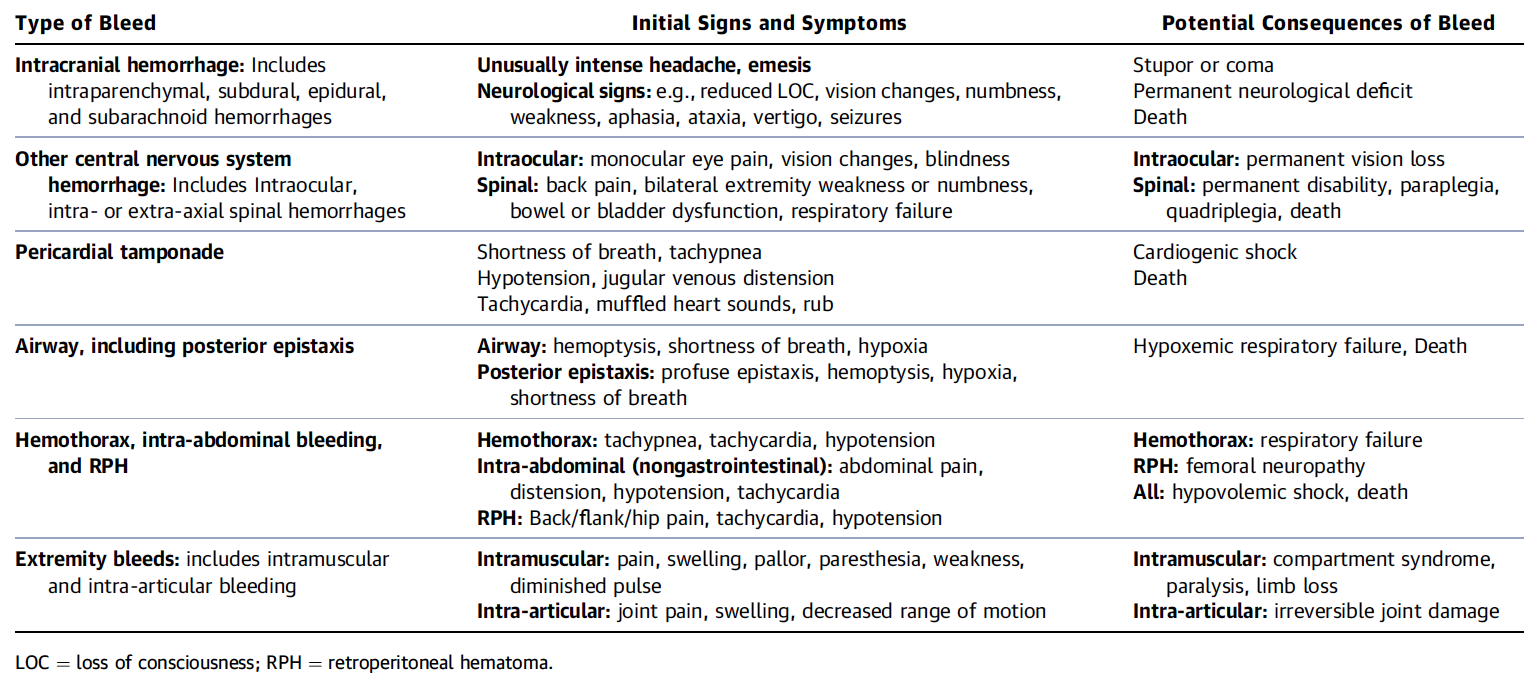
- What is a critical bleed (apart from obvious massive bleeding)? Does this bleeding need imminent reversal?
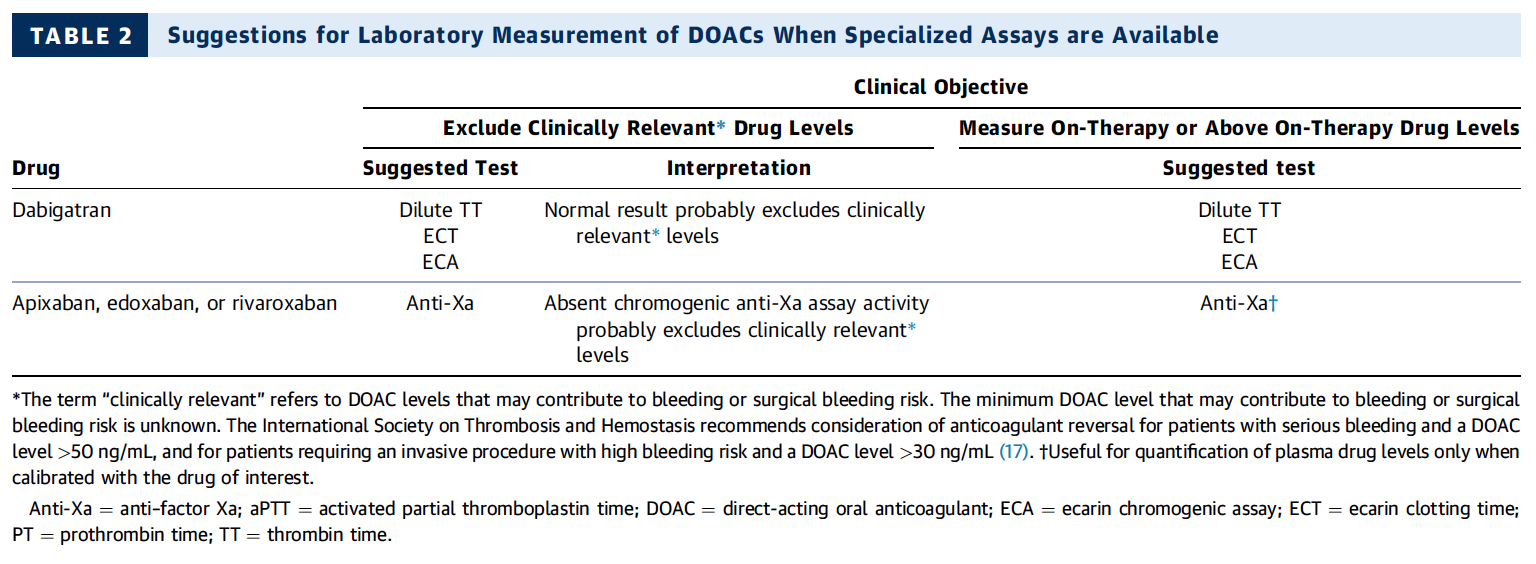
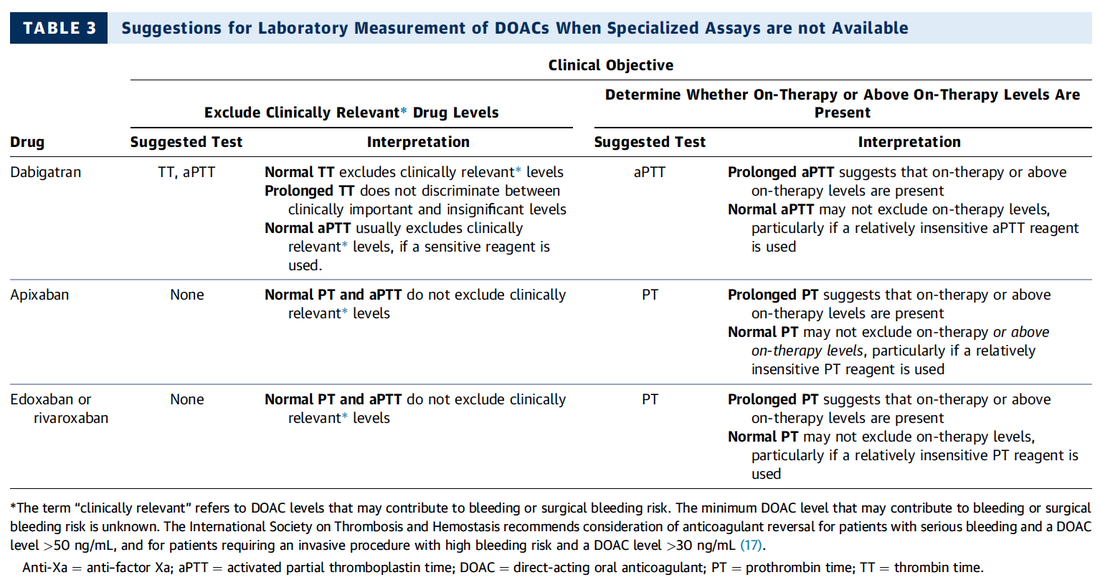
- Do I need any laboratory testing before?
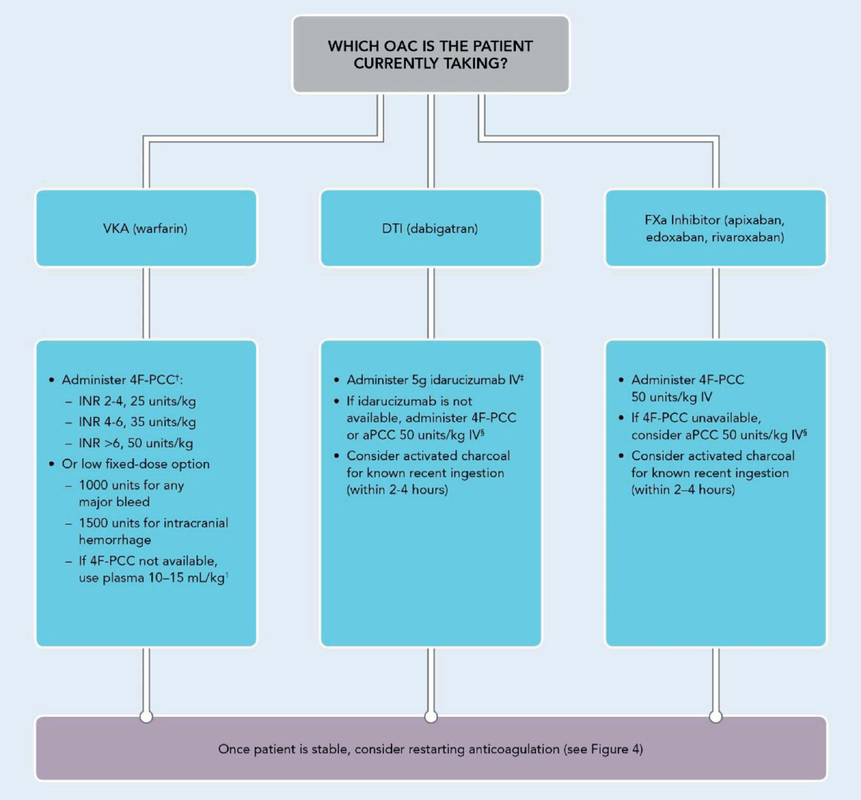
- What treatment should I actually give the patient?
If you do not have a guideline in your institution, it may be time to create one, and the following publication is indeed very useful for this purpose!
The 2017 ACC Expert Consensus Decision Pathway on Management of Bleeding in Patients on Oral Anticoagulants very nicely summarises current evidence and expert opinion on these issues. But the very best are their excellent figures, providing all the answers you need: simple and very understandable!
What is a Critical Bleeding?
Do I Need any Laboratory Tests Before?
What Treatment Should I Give the Patient for Reversal?

The Goodies of Ket
- Has no adverse effects on the gastrointestinal tract (bleeding) and does not cause acute kidney injury (compared to nonsteroidal anti-inflammatory drungs, NSAID's)
- Does not negatively influence bowel motility (in contrast to opioids)
- Preserves laryngeal protective reflexes
- Lowers airway resistance
- Increases lung compliance
- Is less likely to cause respiratory depression
- Is sympathomimetic, facilitates adrenergic transmission and inhibits synaptic catecholamine reuptake, therefore increasing heart rate and blood pressure
The Concerns of Ket
- Might increase pulmonary airway pressure and therefore aggravate pulmonary hypertension
- Might cause well known psychotomimetic effects which are of concern in the critically ill patient as this might predispose to delirium
- Interacts with benzodiazepines via the P450 pathway which could result in drug accumulation and prolonged recovery
Concerns Proven Wrong
- Current evidence shows no increased intracranial pressure or associated adverse neurologic outcomes associated with ketamine administration in critically ill patients
Take Home
Taking precautions and contraindications into account ketamine is considerably safe and even avoids potentially adverse side effects of other agents used.
Erstad BL, J Crit Care, Oct 2016, Vol 35, p 145-149
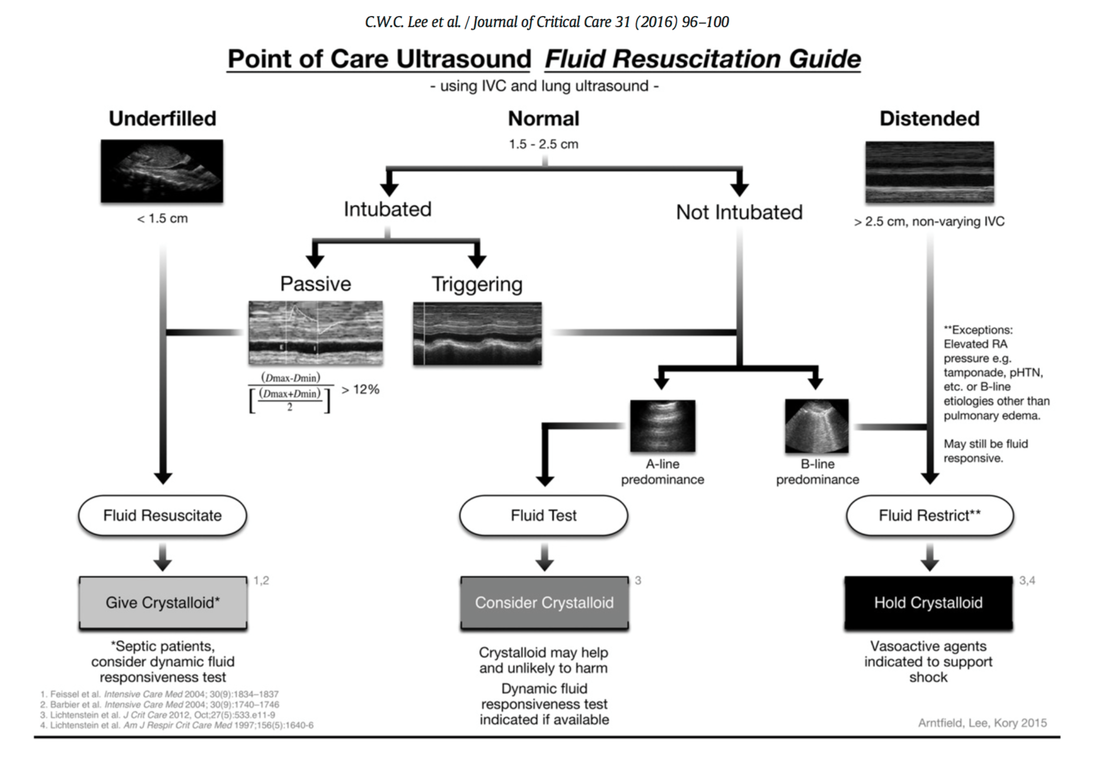
In this regard the use of point-of-care ultrasound (POCUS) has become increasingly attractive in order to use basic critical care ultrasound to asses the need of fluids in a specific clinical setting. Lee at al. have now looked at the sonographic assessment of the inferior vena cava and lung ultrasound in order to quite fluid therapy in intensive care. By taking into account current evidence they have produced an algorithm using these measures to help guiding fluid therapy.
As with any measurement in critically ill patients the pathophysiologic cause of shock must be taken into account. The algorithm presented here seems to work best in patients in hypovolemic shock. To fully understand the following algorithm and its limitations we recommend to read the open access article (see link below).
In conclusion:
The algorithm provided is a helpful tool to help assess the need of fluids in a simple and quick manner.
Lee C et al. J of Crit Care 31 (2016) 96-100 OPEN ACCESS

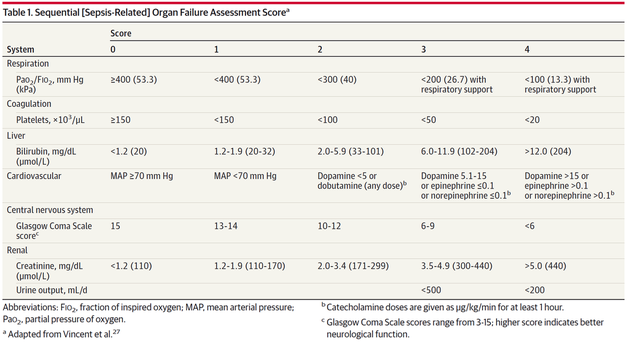
The New Approach to Sepsis - The SOFA
The new international consensus definitions for sepsis and septic shock try to focus on the fact that sepsis itself defines a life-threatening organ dysfunction caused by a dysregulated host response to infection. By saying this the aim is to provide a definition that allows early detection of septic patients and allow prompt and appropriate response. As even a modest degree of organ dysfunction is associated with an increased in-hospital mortality the SOFA score (Sequential or 'Sepsis-related' Organ Failure Assessment) was found to be the best scoring system for this purpose. It's well known, simple to use and has a well-validated relationship to mortality risk.
Sepsis (related organ dysfunction) is now defined by a SOFA score increase of 2 points or more
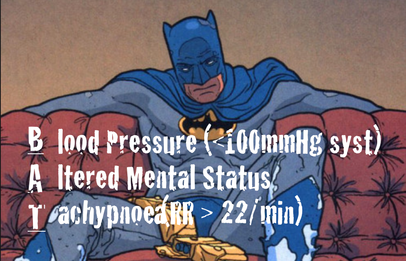
The Quick Approach to Sepsis - The BAT
In the out-of-hospital setting, on the general wards or in the emergency department the task force recommends an altered bed side clinical score called the quickSOFA - or alternatively 'the BAT' score:
The New Approach to Septic Shock -Vasopressors and Lactate
Septic shock is now defined as a subset of sepsis in which underlying circulatory, cellular, and metabolic abnormalities are associated with a greater risk of death than sepsis alone. Keeping a long story short:
Septic Shock is now:
- The need for vasopressors to maintain a mean arterial pressure of at least 65mmHg
AND
- a serum lactate level of more than 2mmol/L... after adequate fluid resuscitation
The Bottom Line:
The way it looks like we are left with Sepsis and Septic Shock
Severe Sepsis has vanished and the question remains, whether these new definitions will actually benefit the ones that need it most... our septic patients!
Singer M et al. JAMA. 2016;315(8):801-810.
Seymour CW et al. JAMA. 2016;315(8):762-774.
Shankar-Hari M et al. JAMA. 2016;315(8):775-787.

When reading this article I couldn't help myself putting a special focus on the controversial issue of cricoid pressure (CP) for rapid sequence induction (RSI). This topic has become a major matter of debate as scientific evidence of its effect on preventing aspiration of gastric content is basically lacking. There is quite some evidence available showing that cricoid pressure might actually impair intubation or potentially harm the patient. More background information and links on this topic you can find here. While some guidelines have actually 'softened' or abandoned the recommendation for the use of CP, most of them have not... and continue to recommend CP. It was therefore of great interest to see what the panel of the DAS would come up with!
For anaesthetists working in Britain and Ireland the DAS guidelines are of special interest as they represent some sort of legal binding on how to proceed at their daily work. We took a closer look at the new guidelines... and got surprised:
"This (CP) is a standard component of rapid sequence induction in the UK". Ok... so no change there! This statement is pretty clear and leaves no space for interpretation - sounds imperative. A little less clear are the following text passages on why CP remains a standard component.
"It is often overlooked that cricoid pressure has been shown to prevent gastric distension during mask ventilation and was originally described for this purpose"... Well, actually cricoid pressure was originally described by Brian Arthur Sellick in the Lancet in 1961 as a preliminary report of an un-controlled case study and the purpose of cricoid pressure was to control regurgitation of gastric content during induction of anaesthesia.
CP and Gastric Insufflation
The reference cited in the context of gastric insufflation and cricoid pressure is an article by Salem and Sellik form Anaesthesia and Analgesia in 1974 (read the original article here). They write: one aim of CP is the prevention of aspiration. The other one is the prevention of gastric insufflation during mask ventilation. The presented evidence in that regard though is not really convincing:
a) A historical letter of Dr. William Cullen... dated back in 1774!
b) The other reference is an article by Salem himself on the 'efficacy of cricoid pressure in preventing gastric inflation during bag-mask ventilation in paediatric patients, but not adults!
Another article cited by the DAS (Obstetric Anaesthetists' Association/Difficult Airway Society difficult and failed tracheal intubation guidelines – the way forward for the obstetric airway Br. J. Anaesth. (2015) 115 (6): 815-818) actually recommends gentle ventilation with low insufflation pressure during RSI which should not overcome correctly applied cricoid pressure. This suggests that CP makes gentle bag-mask ventilation safe.
Indeed, Lawes et al. already showed in 1987 that when bag-mask ventilating, it was not possible to cause gas to enter the stomach in any patient with a patent airway when cricoid pressure was applied. BUT he also stated that: In the absence of cricoid pressure the lungs of all the patients could be ventilated “gently” satisfactorily by hand without gas entering the stomach.
The Bottom Line
Going through these overall brilliant guidelines by the DAS I still haven't been convinced about the usefulness of cricoid pressure and resume (once again):
- Cricoid pressure for rapid sequence induction remains a non-evidence-based manoeuvre and should be seriously questioned!
And by the way, I feel the DAS actually knows that. You have to acknowledge what Hagberg writes in the BJA editorial:
..."the application of CP during rapid sequence induction remains a matter of debate; some believe in its effectiveness in preventing pulmonary aspiration, whereas others believe it should be abandoned because of the paucity of scientific evidence of benefit and possible complications."
..."The literature does demonstrate that the use of CP is likely to make airway interventions, such as mask ventilation, SGA insertion, direct laryngoscopy, and intubation more difficult."
..."As a result of the lack of sufficient scientific evidence that CP reduces regurgitation, in addition to evidence that it may interfere with airway management..."
Any comments?
Difficult Airway Society DAS 2015 guidelines for management of unanticipated difficult intubation in adults, Br. J. Anaesth. 2015 OPEN ACCESS
BIJC post on Cricoid Pressure 04/2014
Hagberg et al. DAS 2015 Guidelines - Editorial, Br. J. Anaesth. 2015, 1-3 OPEN ACCESS
Lawes et al. Inflation Pressure, Gastric Insufflation and Rapid Sequence Induction, Br. J. Anaesth. 1987
OUT NOW: New and Updated ILCOR 2015 Treatment Recommendations on Cardiopulmonary Resuscitation
23/10/2015

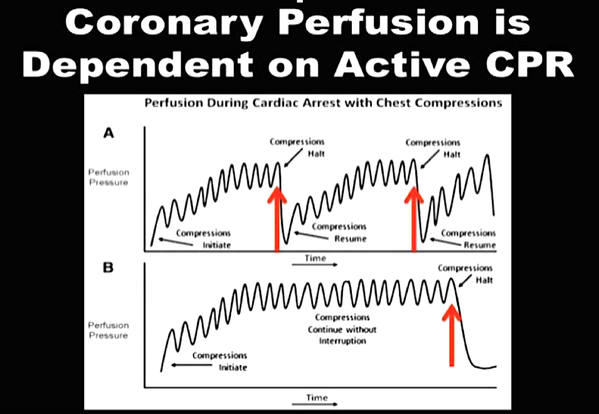
Resuscitation remains one of the most challenging situations in health care. Providing basic and advanced cardiac life support gives you the opportunity to virtually safe a patients life but in a very limited period of time. It is an enormous challenge to consider all emerging evidence and pack this into simple and useful guidelines.
It is imperative to for any health care provider to get familiar with the updated guidelines and major changes. Below you can find all relevant links to get the reading going.
The team of BoringEM.org in Canada have provided some excellent infographics to visualise all important changes in the new treatment guidelines since 2010. You should also note that the Canadian Heart & Stroke Association and the American Heart Association have just published the 'HIGHLIGHTS of the 2015 American Heart Association Guidelines Update for CPR and ECC', an excellent summary of the new recommendations and changes. So if you can't find the time to read all of the publication in 'Circulation', this will certainly provide all information you need to know.
Summary of the Canadian Heart & Stroke Association and the American Heart Association: HIGHLIGHTS of the 2015 American Heart Association Guidelines Update for CPR and ECC
The original publication in Circulation, October 20, 2015, Volume 132, Issue 16 suppl 1
OPEN ACCESS
The Most Important Changes (Click to Enlarge)
The Updated Algorithms (Click to Enlarge)
ERC and ESICM 2015 Guidelines for Post-Resuscitation Care
Nolan JP, Resuscitation, October 2015, Pages 202 - 222

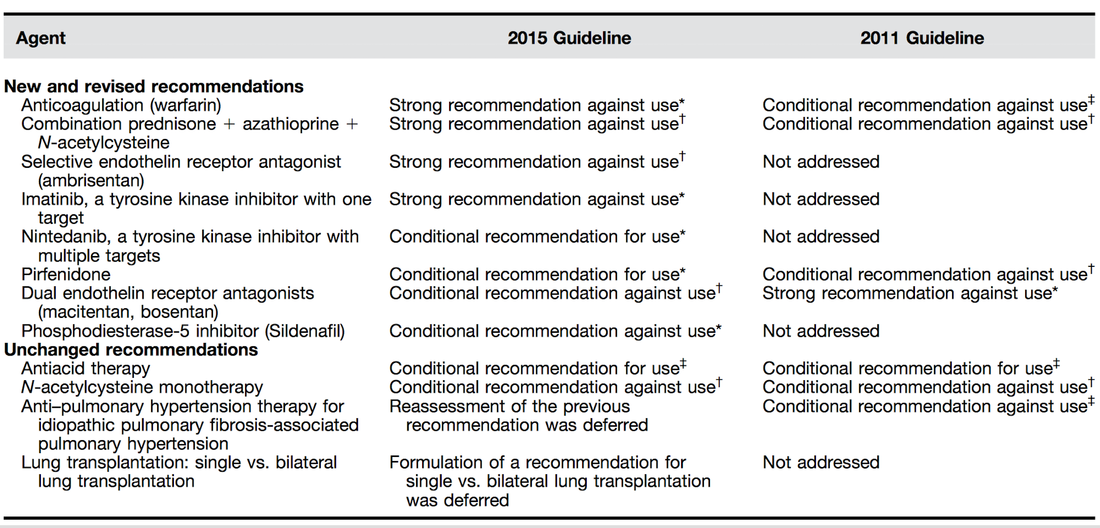
As knowledge is growing the ATS, ERS, JRS and ALAT (... thoracic and respiratory societies) made the effort to look into the latest evidence by performing systematic reviews and where appropriate meta-analyses. The aim was to update the guidelines published in 2011. These guidelines are also dedicated to Mr. William Cunningham who actively participated in the development of these guidelines, suffered from idiopathic pulmonary fibrosis for many years and who was directly confronted with the issues related with this condition.
The main conclusions can be briefly summarised as follows:
An Official ATS/ERS/JRS/ALAT Clinical Practice Guideline: Treatment of Idiopathic Pulmonary Fibrosis. An Update of the 2011 Clinical Practice Guideline, American Journal of Respiratory and Critical Care Medicine, Vol. 192, No. 2 (2015), pp. e3-e19.
OPEN ACCESS: Executive Summary 2015
An Official ATS/ERS/JRS/ALAT Statement: Idiopathic Pulmonary Fibrosis: Evidence-based Guidelines for Diagnosis and Management, Am J Respir Crit Care Med Vol 183. pp 788–824, 2011 OPEN ACCESS
For further information on acute exacerbations of IPF we recommend this Review Article:
| Acute Exacerbations in Patients with IPF,Kim Respiratory Research 2013, 14:86 | |
| File Size: | 321 kb |
| File Type: | |

The authors look at this topic point for point and review current literature in an easy to understand sort of manor. They define major blood loss when it leads to a heart rte of >110/Min or a systolic blood pressure of less than 90mmHg, or simply said: when bleeding becomes haemodynamic relevant. In general it is recommended to have a major haemorrhage protocol at hand (1D) and all staff should be trained to recognise major blood loss early (1D).
Here's a summary of the recommendations made by the British Committee for Standards in Haematology (BCSH):
In Major Haemorrhage....
Red Blood Cells RBC
- Hospitals must be prepared to provide emergency Group 0 red cells and group specific red cells (1C)
- Patients must have correctly labelled samples taken before administration of emergency Group 0 blood (1C)
- There is NO indication to request 'fresh' or 'young' red cells (under 7d of storage, 2B)
- Note: The optimum target haemoglobin concentration (Hb) in this clinical setting in general is NOT established. Current literature shows a tendency towards restriction towards 70-90g/L, but the BCSH makes no recommendations therefore (see blow)
Cell Salvage (e.g. cell saver)
- 24h access to cell salvage should be available in cardiac, obstetric, trauma and vascular centres (2b)
Haemostatic Monitoring
- Use haemostatic tests regularly during haemorrhage, every 30-60min, depending on severity of blood loss (1C)
- Measure platelet count, PT, aPTT (1C)
- Note: The BCSG does not recommend TEG and ROTEM at this stage
Fresh Frozen Plasma FFP
- Use FFP in a 1:2 ratio with RBC initially (2C)
- Once bleeding is under control administer FFP when PT and/or aPTT is >1.5 times normal (recommended dose 15-20ml/kg, 2C)
- The use of FFP should not delay fibrinogen supplementation if necessary (2C)
Fibrinogen
- Supplement fibrinogen when levels fall below 1.5g/L
Prothrombin Complex Concentrates PCC
- Do not use PCC
Platelets
- Keep the platelet count >50 x 10^9/L (1B)
- If bleeding persists give platelets if count falls below 100 x 10^9/L (2C)
Tranexamic Acid TA
- Give tranexamic acid as soon as possible to patients with, or at risk of major haemorrhage (Recommended dose: 1g IV over 10min, followed by 1g IV over 8h, 1A)
- Note: TA has no known adverse effects
- Note: Aprotinin is not recommended
Recombinant Activated Factor VIIa (Novo Seven)
- Do not use
Specific Clinical Situations
Obstetrics
- Fibrinogen levels increase during pregnancy to 4-6g/L
- In major obstetric haemorrhage fibrinogen should be given when levels are <2.0g/L (1B)
GI-Bleed
- Use restrictive strategy for RBC transfusion is recommended in most patients (1A)
Trauma
- Transfuse adult trauma patients empirically with a 1:1 ratio of FFP : RBC (1B)
- Consider early use of platelets (1B)
- Give tranexamic acid as soon as possible (Dose 1g over 10min and then 1g over 8h, 1A)
Prevention of Bleeding in High-Risk Surgery
- Use tranexamic acid (Dose 1g over 10min and then 1g over 8h, 1B)
Hunt B et al. British J Haemat, July 6 2015
Read more HERE:
Great Review on Transfusion, Thrombosis and Bleeding Management
Restricitve Transfusion Threshold in Sepsis, the TRISS Trial
Transfusion: Harmful for Patients Undergoing PCI?
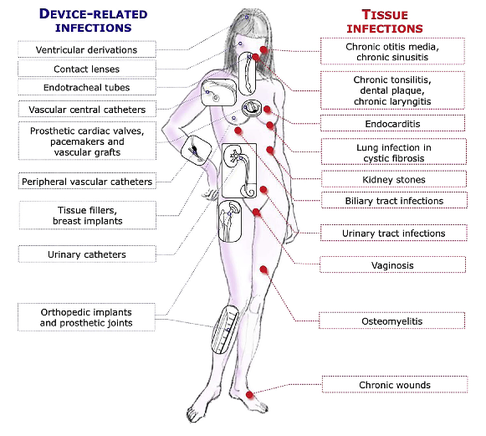
These guidelines outline the nature and properties of biofilms and and their implications on mostly chronic infections caused. As biofilms are very common in critically ill patients it is important to know what specific problems you might encounter, how to proceed and perform a proper diagnosis and what are the essential bits and pieces in the prevention and treatment of biofilm infections.
The article is OPEN ACCESS: Clin Microbiol Infect. 2015 Jan 14. pii: S1198-743X(14)00090-1.
Search
Translate
Select your language above. Beware: Google Translate is often imprecise and might result in incorrect phrases!
Categories
All
Airway
Cardiovascular
Controversies
Endocrinology
Fluids
For A Smile ; )
Guidelines
Infections
Meducation
Neurology
Nutrition
Pharmacology
Procedures
Radiology
Renal
Respiratory
Resuscitation
SARS CoV 2
SARS-CoV-2
Sedation
Sepsis
Transfusion
Archives
January 2021
September 2020
March 2020
February 2020
January 2020
December 2019
November 2019
July 2019
May 2019
March 2019
February 2019
January 2019
December 2018
January 2018
October 2017
August 2017
June 2017
March 2017
February 2017
January 2017
October 2016
July 2016
June 2016
April 2016
February 2016
December 2015
October 2015
September 2015
August 2015
July 2015
June 2015
May 2015
April 2015
March 2015
January 2015
December 2014
November 2014
October 2014
September 2014
August 2014
July 2014
June 2014
May 2014
April 2014
March 2014
February 2014
January 2014
December 2013
November 2013
Author
Timothy Aebi









 RSS Feed
RSS Feed


