Acute myocardial infarction - It's pain radiating to the right arm we have to worry about!15/3/2019
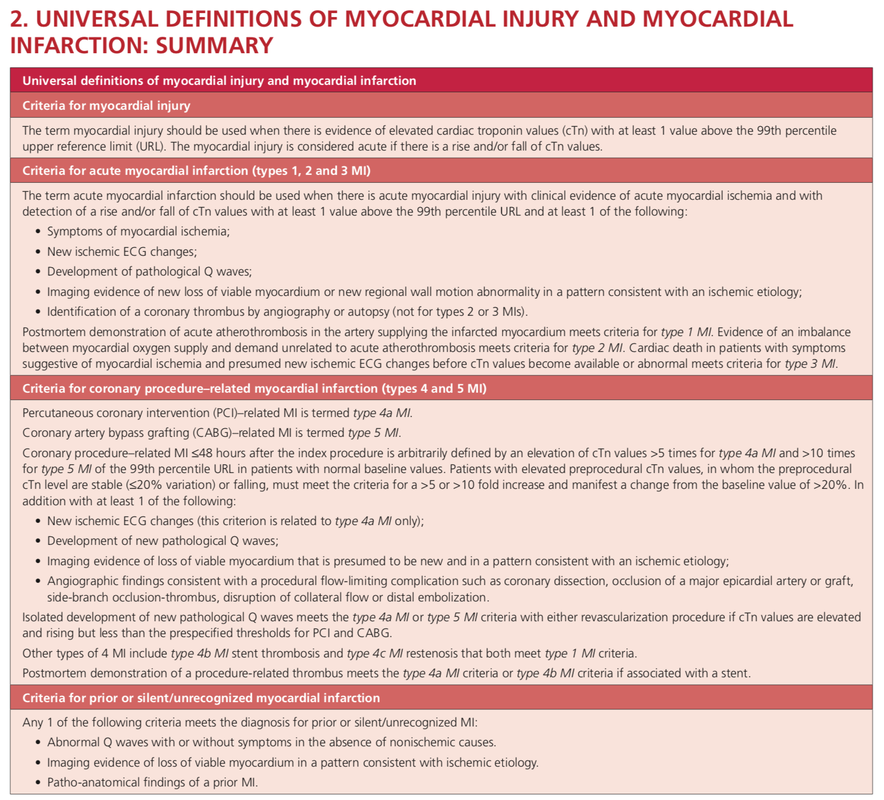
 It was only back in in 1987 when William Heberdeen (not to confound with William Heberdeen, a London doctor who described the Heberdeen nodes back in the 18th century) published the first description of ischemic chest pain. It was the birth of the classical image of strangling chest pain that occasionally radiates to the left arm, associated with exertion and relieved by rest. A recent publication in the BMJ shows, that positive troponin levels are found frequently in patients with non-cardiac problems. This finding underlines the importance of good history taking, including the assessment of chest pain (CP) characteristics.
|
Search
|





















 RSS Feed
RSS Feed


