|
Many rumours are going around about Metamizole; most of them are full of fear of potential side effects. Some countries like Ireland and GB have banned this drug due to the rare side effect of agranulocytosis. A fact is too that many other countries like Switzerland continue to use Metamizole on a regular basis and find low incidence rates of 0.46-1.63 cases per million person-days of use (2006-2012). Regarding serious side effects associated with other analgesics used (e.g. acute liver failure with Paracetamol, renal failure with NSAID) it is difficult to understand why Metamizole needs to be banned when the others are available over the counter. Get all the information AND literature you need to be prepared and discuss here: https://icurevisited.com/dipyrone-metamizole/ This site provides a growing number of reliable FOAM-resources, dedicated to provide expert knowledge for health care professionals. A special section has no been added, that provides many links to COVID-19 specific resources. www.foam.education The amount of publications and current spread of knowledge on the outbreak of the coronavirus is overwhelming. As patient number keeps growing worldwide, almost all health care professionals in critical care are treating patients with coronavirus disease (COVID). It is therefore imperative that protective measures are taken seriously, as infected or even sick hospital staff would complicate the situation even more.
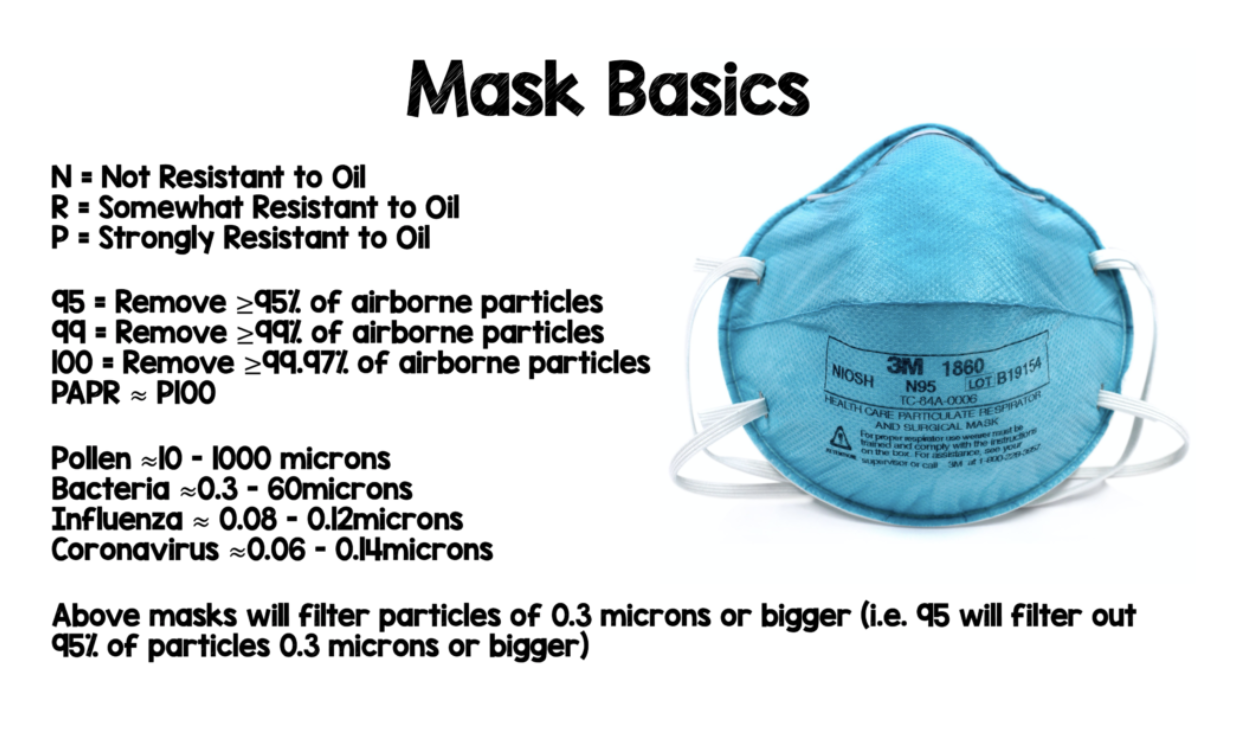
Salim Rezaie from REBEL EM has just recently posted an excellent article on different preventive measures in regards to COVID-19. The main focus of this blog post is on face-masks though:
Don't miss this read, maybe the best one out there: REBEL EM: COVID-19 Prevention Most Swiss Guidelines recommend never to drain more than 1500ml of pleural fluid when performing a thoracocentesis. The reason is that excessive drainage might cause re-expansion pleural effusion (e.g. www.medstandards.ch). There is not much literature on the safe amount of fluid one can drain, but a clinical practice article on pleural effusions in the New England Journal of Medicine also states that "...in which case therapeutic thoracentesis to remove up to 1500 ml of fluid is indicated." (N Engl J Med 2002; 346:1971-1977). Interestingly there is no evidence supporting this recommendation. Some data suggests that the risk of re-expansion pulmonary oedema might correlate with the baseline size of the effusion, rather than the volume of fluid removed. However, the first results from research start giving us some answers and indicate that removing more than 1500ml of fluids is safe and feasible. Ault M et al. (Thorax. 2015;70(2):127-132.) looked at 9320 patients during 11 years who underwent thoracocentesis and recorded the incidence of adverse events. They were able to show that:
Lentz RJ et al. (Lancet Respir Med. 2019;7(5):447-455.) showed that
All the details and lots of background information are very nicely summarized in this fabulous post on emcrit.org: PulmCrit - Large volume thora: Can we drain 'em dry? Reference
1. Reid C, Rees V, Collyer-Merritt H. Non-septic hyperlactataemia in the emergency department. Emerg Med J. 2010 May;27(5):411–2 This is an excellent 5 min video on the proper use of a Linton tube in massive bleeding varices!
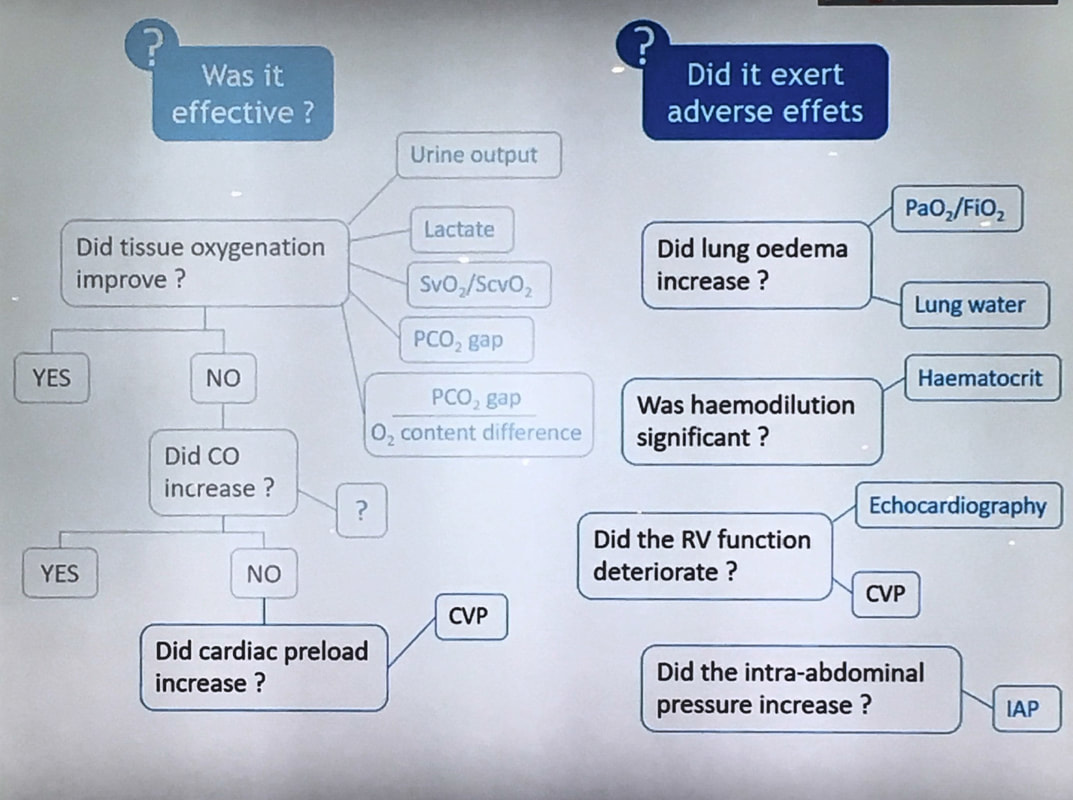
Here's a single slide showing nicely why we measure different values during fluid therapy and what information they provide. Excellent pearl of knowledge shared by Xavier Monnet at #ISICEM2018.
 "The Critical Care Reviews Book summarises, critiques and puts in context the biggest trials of the year." There is not much more to add. Rob Mac Sweeney and four other intensivists of Northern Ireland try to make the impossible - possible. On 344 pages they have summarised a selection of the maybe most relevant trials concerning critical care of 2016. In regards of all the countless trials published every year this is a fantastic piece of work. Supporting the idea of Free Open Access Meducation this book is free for download and a must for any clinician involved in critial care. Great job lads! The free download is available HERE  This excellent post by Josh Farkas from Emcrit.org resumes nicely on how our daily work sometimes is influenced by fears and not knowledge. If you are worried to give a patient meropenem after he had an anaphylactic reaction to penicillin in the past... then this reading is for you! His Bottom Line comes as follows:
Don't miss out this excellent post: PulmCrit mythbusting - Anaphylaxis to penicillins isn’t a contraindication to meropenem |
SearchTranslateSelect your language above. Beware: Google Translate is often imprecise and might result in incorrect phrases!
|


 RSS Feed
RSS Feed


