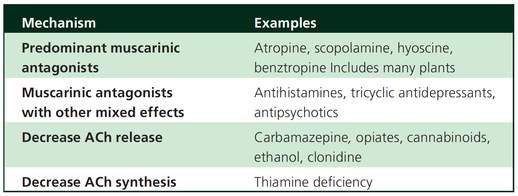
 Just recently a 75-year-old gentleman was admitted to our unit as he remained unresponsive after short procedural sedation with Propofol. Although he was hemodynamically stable and showed proper spontaneous breathing at any time, the intervention team was concerned about his condition. On arrival to our ICU, the patient was noted to be still unresponsive. He showed no reaction to painful stimulation. The Pupils were rather wide, but symmetrical in size and showed a prompt response to light. Brain stem reflexes were present and peripheral reflexes were triggerable. His breathing pattern was regular, and saturation levels were above 96% on room air. A blood gas analysis showed a normal pH and normal CO2-levels. As usual, the common reflexes started to kick in, and some suggested to go for a CT-scan of his head to out-rule some significant complications. Luckily enough, close observation revealed some slow improvement of his alertness, and we considered the possible diagnosis of a central anticholinergic syndrome (CAS). After the application of 1mg of physostigmine (2x0.5mg) intravenously the patient almost promptly awoke and had an uneventful stay on our unit. This case just reminded me of these many patients in anaesthesia that inexplicably show delayed awakening after sedation or a general anaesthetic. In fact, it is estimated that the incidence of central anticholinergic syndrome is around 8- 12 % following general anaesthetic and lesser with regional anaesthesia. What is a Central Anticholinergic Syndrome? Classically the central anticholinergic syndrome (CAS) describes a condition where a substance causes a competitive antagonism of acetylcholine (ACh) at peripheral and central muscarinic receptors. Initially, these were plants containing atropine, hyoscyamine and scopolamine. There are four muscarinic receptors: - M1 mainly in the central nervous system (responsible for delirium when antagonised) - M2 in the brain and heart - M3 in the salivary glands and - M4 in the brain and lungs The PERIPHERAL SYNDROME presents with: - Dry mouth - Difficulty swallowing (lack of saliva) - Photophobia and blurred vision (due to dilated pupils) - Dry skin, fever - Reduced bowel sounds and urinary retention The CENTRAL SYNDROME presents with: - Agitation, agitated delirium, visual and auditory hallucinations - Hypoactive delirium may also occur, this seems to be more common though in the postoperative setting The clinical diagnosis of a CAS is more straightforward when typical peripheral symptoms accompany central signs. The Problem with the "Silent" Postoperative CASThe clinical diagnosis of a CAS is often straight forward when typical central symptoms accompany peripheral symptoms. The problems are patients in the postoperative setting, in which the patient often presents with somewhat atypical central symptoms and often minimal or even no peripheral symptoms at all. Especially in this setting, the anticholinergic syndrome may be accompanied by sedation or coma. The mechanisms causative for this phenomenon are not well understood but might include greater tolerance at peripheral receptors, longer persistence at central receptors or greater CNS susceptibility due to age or disease. Postoperative CAS is often associated with atypical central symptoms and minimal or even no peripheral signs at all! Sedation and coma are often observed in this setting. What Drugs Cause CAS?Common anticholinergics agents should be more accurately referred to as antimuscarinics, as these agents do not generally block nicotinic receptors. The Problem is that many currently used drugs in anaesthesia and critical care are also known to cause this syndrome. This includes: Benzodiazepines, opioids, phenothiazines, butyrophenones, ketamine, etomidate, propofol, nitrous oxide, and volatile inhaled anaesthetics! How Can I Diagnose a "Silent" Postoperative CAS?The fact that postoperative CAS often lacks the presence of peripheral symptoms makes the diagnosis challenging. The different presentation of the syndrome ranging from somnolence, confusion, amnesia, delayed recovery, stupor, coma to agitation, hallucinations, dysarthria, ataxia, delirium makes it difficult to diagnose accurately. It is, therefore, a diagnosis of exclusion! The most helpful tool you have is physostigmine! The prompt arousal of a patient after the application of intravenous physostigmine is highly suggestive of a postoperative central anticholinergic syndrome. How to Use PhysostigmineWhen dealing with prolonged somnolence or unexplained agitation following any form of anaesthesia, make sure to check and monitor vital signs and provide basic or advanced life support if necessary. Exclude common causes first (e.g. overhang of sedatives or opioids, persistent muscular paralysis, hypoxemia, hypercapnia, hypoglycemia and other). If common causes can be excluded and CAS is a probable diagnosis, you should consider the application of intravenous physostigmine. Physostigmine in recommended doses is considered safe! Possible adverse effects are considered unlikely. Studies found cholinergic symptoms sometimes to be mild, and these adverse effects are more an indication of probable excessive doses rather than an established safety concern. For postoperative CAS a dose of 1mg of physostigmine i/v is recommended. This dose can be divided into two doses of 0.5mg i/v if required. The maximum dose recommended in this setting is 2mg i/v.  Beware: You are giving Physostigmine Salicylat - Do not give to patients with aspirin allergy! |
Search
|



 RSS Feed
RSS Feed


