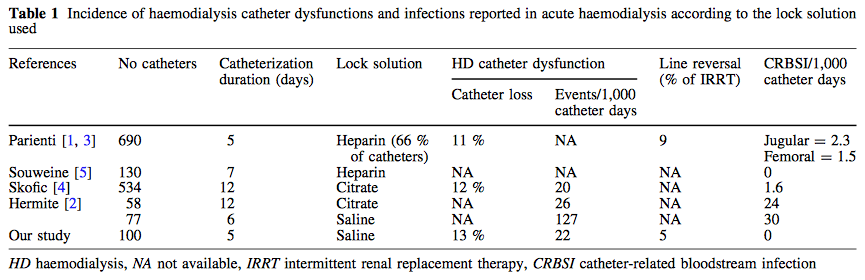
 Antibiotic-associated diarrhoea and antibiotic induced Clostridium difficile diarrhoea are a constant problem in the ICU, especially in the elderly patient. There is still some debate going on about prescribing lactobacilli or bifidobacteria for the prevention and treatment of this sort of complication. In this Lancet multi centre, randomised, double-blind, placebo-controlled, pragmatic, efficacy trial this was studied on almost 3000 patients: 10.8% diarrhoea with lactobacilli or bifidobacteria versus 10.4% diarrhoea in the placebo group. No difference! One drug less to prescribe... Lancet 2013 Oct 12;382(9900):1249-57  In a letter to the editor of Intensive Care Medicine Soubirou et al. present the result of a study looking at the efficacy and safety of saline lock solution in maintaining short term hemodialysis catheters patency in ICU. This prospective cohort study looked at 100 double lumen hemodialysis catheters inserted in 75 patients managed with intermitted hemodialysis. At the end of each session the lumens were flushed with normal saline only. The investigators found no difference to 5 other studies using heparin or citrate. Conclusion: Heparin is not necessary in this setting, citrate is an alternative, but saline seems just as good. Soubirou JF et al. Intensive Care Med. 2014 June  Not only the detection but also the treatment of airway pathogens has become a major problem in intensive care units. As mentioned by the WHO multi drug-resistant organisms are a problem and will have a great impact on our clinical work in the future. In all the discussions on restricting antibiotic usage and infection control comes this article by Palmer et al. where they look at actually reducing antibiotic resistance by using antibiotics - Inhaled antibiotics. In itself actually a breach of paradigm. In a double-blind placebo-controlled study including a rather small group of critically ill intubated patients they found that aerosolised antibiotics successfully eradicated existing multi-drug resistant organisms and therefore reduced the pressure from systemic agents for new resistance. While this article is not open access, the editorial by M. Bonten is. Palmer LB et al. Am J of Resp and Crit Care Med, Vol. 189, No. 10 (2014), pp. 1225-1233 MJM Bonten, Editorial, Am J of Resp and Crit Care Med, 2014  This months issue of the American Journal of Respiratory and Critical Care Medicine presents a retrospective cohort study comparing patients with acute exacerbation of COPD receiving either lower-dose methylprednisolone (<240mg/d) or high-dose methylprednisolone (>240mg/d). They looked at 17'239 patients. The primary outcome was mortality. Despite the possibility of some selection bias they conclude that high doses of methylprednisolone are associated with worse outcomes and more frequent adverse effects (like prolonged hospital and ICU length of stay, higher hospital costs, increased length of invasive ventilation, increased need for insulin therapy and higher rate of fungal infections). Mortality itself did not significantly differ. It is remarkable to note that in this study doses below 240mg of methylprednisolone are considered low-dose. This is equivalent to 300mg of prednisolone and is relatively high for exacerbations of COPD. As we mentioned in a post in November 2013 the REDUCE trial in JAMA compared 5 days to 14 days of steroids in exacerbated COPD. The dosage used there was 40mg of prednisone. The results showed that a 5-day treatment was non-inferior to a 14-day treatment with regard to re-exacerbation within 6 months but significantly reduced glucocorticoid exposure. In summary it seems to be advisable to use lower doses and short treatment periods in acute exacerbated COPD. Am J Respir Crit Care Med. 2014 May 1;189(9):1052-64 Simply Great and Helpful: Normogram for Calculating the Maximum Dose of Local Anaesthetics20/5/2014
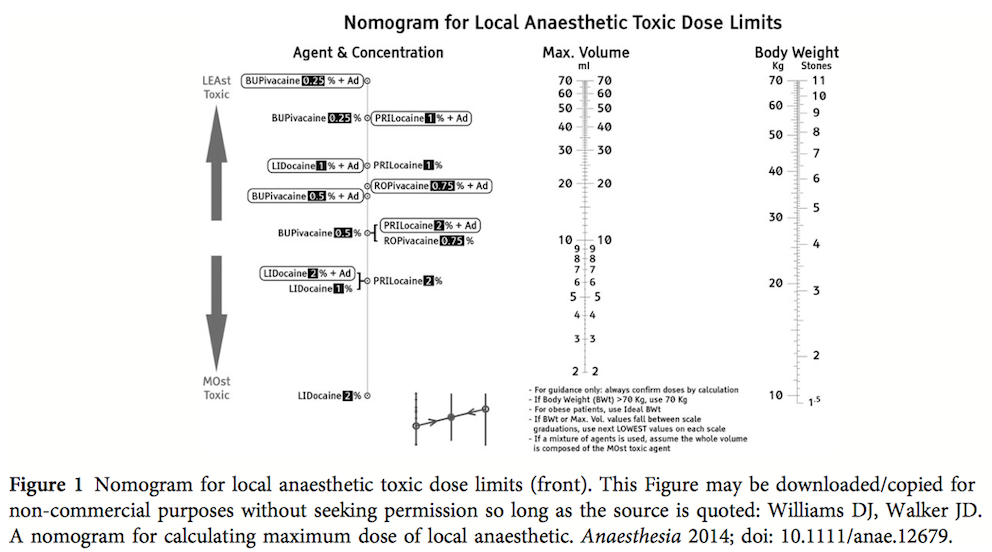
 While many medical articles conclude 'more research is needed...', or further study is required' here comes a straight forward article that gives you a simple, but very helpful tool for your daily work. In this month's Anaesthesia Williams and Walker present a normogram for calculation of the maximum safe volume (ml) of local anaesthetic to a clinical acceptable degree of accuracy. Indeed this normogram allows you to find out the various doses within a few seconds. In their article they looked at 14 commonly used local anaesthetics and provide some further background information. The normogram only works with body weights up to 70kg, but they recommend to use the ideal body weight for obese patients. An article worth reading (open access!) and a normogram worth using! Williams DJ et al. Anaesthesia. doi: 10.1111/anae.12679 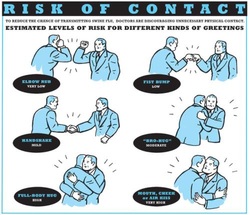 After the 2013 publication by Ghareed et al. (see BIJC post here) on fist bumps in the health care setting in order to prevent transmission of pathogens JAMA now joins in the discussion. Sklansky M et al. published a viewpoint on the banning of the handshake from the health care setting. In their paper they point out that the hands of health care workers often serve as vectors for transmission of organisms and disease. The fact is highlighted that adherence of health care providers with hand hygiene remains rather low and that handshakes have shown to be able to transmit pathogens. In their article they draw parallels between the ban of handshakes in a health care setting and the ban of smoking in public places and finally offer a variety of alternative greetings methods like: the 'hand wave' and placement of the right palm over the heart, or the Namaste gesture also practiced in yoga around the world. This offers an interesting viewpoint worth reading indeed but I might add a few remarks and questions to this article. Apart from the fact that I still struggle to follow the link between hand shakes and smoking in public and would like to highlight following: - The link between pathogen transmission by handshakes and consecutive patient outcome is totally unclear. At this stage there is no evidence indicating that handshakes themselves impose a serious threat to patients. - Banning handshakes in hospitals might sound like a good idea, but the main problem remains unaffected. Multi-resistant bacterias are the logical result of inappropriate prescription and usage of antibiotics. It certainly is advisable to prevent the spread of these pathogens but it would be better to prevent their man made evolution. - Physical contact with patients in the ICU is an essential part in patient care (e.g. nursing or medical examination) and socialising might be even more important when you're unwell. Of course contact isolation has been found to help prevent the retransmission of pathogens. We tend to forget though that all these measures at the same time might have other unintended consequences. From 1999 to 2003 three articles showed that patients in contact isolation got half as many visits from health care providers resulting in 20% less contact time (Morgan DJ et al. Infect Control Hosp Epidemiol. 2013;34(1):69-73). Remarkably, similar effects were found also a decade later. Evidence has continued to accumulate that patients on contact precautions may experience worse outcomes, including more delirium, more depression, worse discharge instructions, and less smoking cessation counselling. Withholding a handshake sounds simple but might actually further contribute to patient's isolation and there is also some research out there actually showing on how important this gesture actually might be (Dolcos S et al. J Cogn Neurosci 2012 Dec;24(12):2292-305). The first sentence of the Conclusion by Sklansky et al. reads as follows: 'Banning the handshake from the health care environment may require further study to confirm and better describe the link between handshake-related transmission of pathogens and disease.'... I couldn't agree more! I think we might have to be very careful on already starting to talk about 'hand shake free zones' as long as there are so many unanswered questions. Many things have been done in the past to prevent infections and finally have been proven to be completely inutile (e.g. changing peripheral lines after three days, read post here). Maybe we she focus more on avoiding overprescribing antibiotics instead. What do you think...? Sklansky et al. JAMA. Published online May 15, 2014. doi:10.1001/jama.2014.4675 The picture displayed above is take from the New York Times  A situation often encountered in hospitals... also in Ireland. You have to urgently review a patient on the ward but are stuck in theatre. Of course you would like to get changed first (as hospital policy asks you to) but there are no scrubs available anymore or there are no white coats to cover your scrubs, or ... so you end up going to the ward in your scrubs... as a walking threat to patients? Apart form the fact that changing your clothes might be appropriate to do there is this recent article of Hee at al. in Anaesthesia giving you a little chance for forgiveness. Although small in numbers these researches found no evidence that visits to ward or office significantly increase bacterial contamination of scrub suits. Hee HI et al. Anaesthesia April 18 2014 Picture above taken from the US series 'Scrubs'  The amino-acid glutamin seems to play an important role in the critically ill patient by inducing cellular protection pathways, modulation of the inflammatory response and the prevention or organ injury. Glutamine depletion on ICU admission has been linked with increased mortality and clinical trials form the last 20 years demonstrated reduced mortality, infectious complications and ICU/hospital length of stay when giving glutamine. This is one of the reasons ICU's give glutamine when total parenteral nutrition (TPN) is required. ...sounds like all ICU patients should get glutamine! In April 2013 the NEJM published a randomised trial of glutamine and antioxidants in critically ill patient by Heyland et al. Against their expectations they found a trend towards increased mortality at 28 days among patients who received early glutamine intravenously and enterally as compared to those who did not. Actually, the early provision of glutamine did not improve clinical outcome and glutamine was associated with an increase in mortality among critically ill patients with multi-organ failure. ... so should we stop giving glutamine? In April 2014 now Heyland and his co-authors (the same guy from the NEJM paper) published a systematic review in Critical Care. In this paper they looked at 26 publications on parenteral glutamine supplementation in the ICU and could actually show that in conjunction with nutrition support glutamine was associated with a significant reduction in hospital mortality and hospital length of stay. They stated that parenteral glutamine supplementation as a component of nutrition support should continue to be considered to improve outcomes in critically ill patient. ... that all seems confusing and contradicting! Actually all these papers aren't conflicting at all. They offer a differentiated insight into the usage of glutamine... the answer lies in the written details of the study settings. Heylands publication in the NEJM presents a quite different setting compared to most of the previous studies where glutamine was found to be rather beneficial. In the NEJM's publication patients received the highest dose of glutamine (more than in other studies before) which was given intravenously and enterally. This study specifically included critically ill patients with multi-organ failure, most of them in shock. In most previous studies this was an exclusion criteria. Also treatment with glutamine was initiated within 24h after admission to ICU, whereas other studies gave glutamine later in the course of disease together with TPN. And finally all these patients received enteral nutrition, while previous studies mostly focused on parenteral nutrition (TPN). And finally, Heyland (again) just now published a post hoc analysis of the NEJM publication in the Journal of Parenteral & Enteral Nutrition (JPEN) showing that early administration of high-dose glutamine separately from artificial nutrition had the greatest potential to be harmful in patients with multi-organ failure that included renal dysfunction. For these reasons Heyland came to the conclusion that early administration of glutamine in critically ill patients with multi-organ failure was harmful. At the same time it seems beneficial when given after resolution of shock especially in the conjunction with TPN. Summarized: - Early administration of high-dose glutamine in critically ill patients with multi-organ failure may be harmful, especially in conjunction with renal dysfunction - Supplemental glutamine (predominantly as a component of TPN) may improve clinical income when given to appropriate patients and after resolution of multi-organ failure and shock - Supplemental glutamine should not be given in high dose (>0.5 g/kg/d) Wischmeyer PE, Critical Care 2014,18;R76 Qi-Hong C, Critical Care 2014,18;R8 Heyland D, N Engl J Med 2013;368:1489-97 Heyland D, J Parenter Enteral Nutr, May 5 2014 One of the Big Mysteries Solved: How to Correctly Prescribe the Duration of Antibiotic Treatments2/5/2014
 Just this week the World Health Organisation WHO has issued a warning that resistance of organisms to antibiotics will become one of the biggest challenges of the upcoming decade. Indeed, the correct prescription of antibiotics is crucial for successful treatment and the WHO states that completing the full length of the treatment is just as important. But what is actually the correct length of treatment for all the different antibiotics and diseases? How many ward rounds on ICU's have I spent with microbiologists (the maybe most important specialists on our sides!) wondering on how they always had a straight answer on the correct length of treatment. 7 days, 10 days or sometimes 21 days... a little mystery to most intensivists, until now! Hitchhiking though the the wide space of the internet I finally found secret to this question. Back in the year 2010 Paul E. Sax, a Professor of Medicine at Harvard Medical School him self, posted an excellent blog for the NEJM Journal Watch website. Inspired by a New York Time article by Harvard Professor Daniel Gilbert he finally gave insight into one of the great mysteries of medicine: To figure out how long antibiotics need to be given, use the following rules:
That did not occur by chance Wow, not much more I can add! Paul E. Sax, NEJM Journal Watch HIV/AIDS Clinical Care, October 22nd 2010 NYT article by Daniel Gilbert from October 2010 |
Search
|


 RSS Feed
RSS Feed


