 Thoracocentesis is a procedure often used to further determine pleural effusions. This commonly performed procedure may lead to complications including the development of a pneumothorax. Wilcox et al. performed a systematic review in JAMA of current literature to answer following two questions: 1. What are the most accurate diagnostic indicators to diagnose an exsudate? and 2. What are the most common adverse side effects and factors affecting them? 48 studies were included to answer the first question, while 37 studies were used to approach question number 2. In conclusion: - Light's criteria, pleural fluid cholesterol (<55 mg/dl) and pleural fluid LDH (>200 U/L) levels, and the pleural fluid cholesterol to serum cholesterol ratio (> 0.3) are the best diagnostic indicators for pleural exsudates - Pneumothorax was the most common complication of thoracocetesis (incidence 6%). Chest tube placement was needed in 2% of all procedures. And most impressive: Ultrasound skin marking by a radiologist or ultrasound-guided thoracocentesis were not associated with a decrease in pneumothorax events. ... would you abandon the ultrasound? Wilcox et al. JAMA, June 18, 2014, Vol 311, No. 23  The Lancet has now published the multi-centre study (PROVHILO) which has looked at the role of positive end-expiratory pressure (PEEP) for mechanical ventilation during general anaesthesia. For that reason the PROVE network investigators have included almost 900 patients in a randomised controlled trial who were planned for open abdominal surgery. All patients were ventilated with a tidal volume (Vt) of 8ml/kg. One group received a PEEP of 12 cmH2O and recruitement maneuvres while the other group got alomst no PEEP (<2 cmH2O) and no recruitement maneuvres. Primary endpoint were pulmonary compications on day 5 postoperatively. They found no difference in pulmonary complications but significantly more introperative hypotension and use of vasoactive agents in the higher PEEP group. So the investigators conclude that a higher level of PEEP and recruitment maneuvres do not protect against postoperative pulmonary complications. They actually advise to use low tidal volumes and very low PEEP for intraoperative ventilation. The multicenter study is well designed and performed but some questions remain: Why is PEEP never adjusted to weight? One striking feature is that we all use tidal volumes according to the patients body weight, but interestingly nobody seems to use this adjustement for weight when it comes to PEEP. Using a PEEP of 12 in a small and slim 50kg patient has a different impact compared to a massively obese patient. Is 12 cmH2O too high? A PEEP of 12 can be considered generally high and is not used by most anaesthetists in their daily practice anyway. There was no third arm using intermediate levels of PEEP to answer the question on how these patient might have performed. Why did other trial find differing conclusions? The aspect of different levels of PEEP is interesting as previous studies actually were able to show improved outcome with 'protective' mechanical ventilation. The IMPROVE trial in the NEJM from Augut 2013 compared patients for abdominal surgery ventilated with Vt of 10-12ml/kg and 0 cmH2O of PEEP to patients ventilated with Vt of 6-8ml/kg and 6-10 cmH2O of PEEP. In this multicenter, double blind trial with 400 patients improved outcome and reduced health care utilazation were found in the group 'protectively' ventilated. In june 2013 Anaesthesiology published a prospective randomized small trial with 56 patients undergoing open abdominal surgery for more than 2 hours. This time they compared Vt of 9ml/kg and O PEEP to Vt of 7ml/kg and 10 PEEP. This time 'protective' ventilation with PEEP improved respiratory function but did not affect length of hospital stay. Taking these fact into account I think we remain with following conclusions: - The PROVHILO trial is not reason enough to abandon PEEP for anaesthetic ventilation in theatre - Instead we might have to consider adjusting PEEP to the patients clinical condition (e.g. weight) - There is no evidence currently to recommend routine recruitment maneuvers in theatre The Prove Network Investigators, The Lancet, Early Online Publication, 1 June 2014  Ketamine - a drug with various actions and just as many opinions on it. One concern often mentioned is that ketamine might cause a raise in intracranial pressure (ICP) and therefore is often avoided in this group of patients. In May's Journal of Anaesthesia Wang et al. looked at the existing evidence on this topic. They ended up with 5 trials meeting their inclusion criteria on administration of ketamine and the ICP levels within the first 24h as a primary outcome. To make it short: Ketamine does not increase ICP in comparison to opioids. They conclude that ketamine should not be discouraged on the basis of ICP-related concerns. Wang et al. J Anaesth. 2014 May 24 Early Systematic Coronary Angiography in All Out-Of-Hospital Cardiac Arrests Seems Reasonable9/6/2014
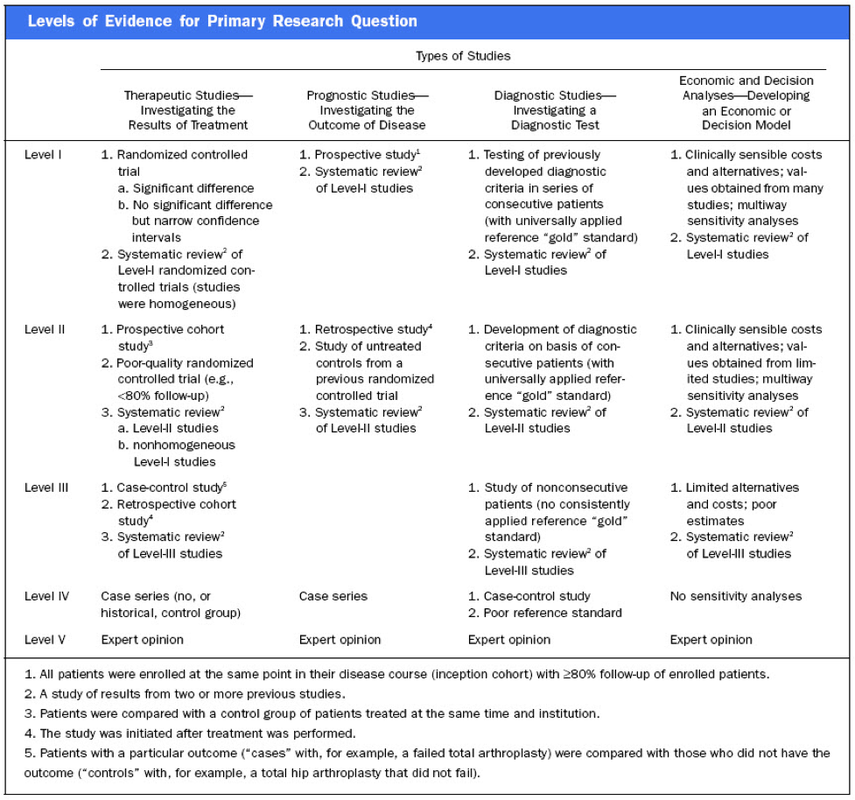
 The most recent guidelines of the European Resuscitation Council and the American Heart Association recommend that resuscitated patients of presumed cardiac cause should undergo immediate coronary angiography with subsequent PCI if indicated, regardless of clinical symptoms and/or ECG criteria. However, this approach is discussed controversially as we don't know if there is any benefit on performing an angiography in every out-of-hospital cardiac arrest (OHCA). Additionally such an approach might be associated with quite some logistical and organisational problems for certain institutions. In this noteworthy and open access review article Geri et al. discuss current literature and state that there are no randomised studies looking at acute coronary angiography in OHCA patients. A large number of observational studies though supports feasibility and a possible survival benefit of an early invasive approach. They conclude that even in the absence of large randomised studies, it is probable that an early coronary revascularization is associated with a significant clinical benefit in OHCA survivors. Providing the patient had no other obvious reason for OHCA (sepsis, haemorrhage, metabolic disorder etc.) current literature strongly encourages performing a systematic coronary angiography in all OHCA patients. Geri G et al., Current Opinion in Critical Care, June 2014, Vol 20, Issue 3 (Open Access)  In the most recent edition of 'Continuing Education in Anaesthesia, Critical Care and Pain' there is a very good overview article on rapid sequence induction (RSI) and its place in modern anaesthesia. Wallace and McGuire also critically look at cricoid pressure (CP) as a part of classical RSI. In their publication they state that "there have been no prospective randomized clinical studies performed to prove the clinical hypothesis and the level of evidence to support the use of cricoid pressure is poor (Level 5)". Level 5 corresponds to 'Expert Opinion' (see table below). They also mention that aspiration has occured despite CP, that CP is often poorly performed, that it may hinder bag-valve mask ventilation as well as LMA insertion and that is may worsen laryngoscopy. It's mentioned that "Critically, it has also been shown to potentially obstruct the upper airway and reduce time to desaturation". 'This is nothing new' you might say. Why am I mentioning this? Well, the remarkable thing about this article is the fact that it was published in a Journal that is a joint venture of the British Journal of Anaesthesia BJA and The Royal College of Anaesthetists in collaboration with the Intensive Care Society and Pain Society. Considering the fact that The NAP4 guidelines continue to support its use as part of an RSI and as such, it is still considered a standard of care in the UK and therefore also Ireland, this publication might indicate some change in mind... or not? The authors summarize: Application of cricoid pressure is advisable — unless it obscures the view at laryngoscopy or interferes with manual ventilation or supraglottic airway device placement. I personally still would want to know what exactly makes a 'Level 5' medical intervention 'advisable' especially in regards of all the possible problems and complications associated with it. Wallace et al., Continuing Education in Anaesthesia, Critical Care & Pain, Volume 14(3), June 2014, p 130–135 Read our previous BIJC post: Cricoid Pressure for RSI in the ICU: Time to Let Go? (Updated) |
Search
|


 RSS Feed
RSS Feed


