|
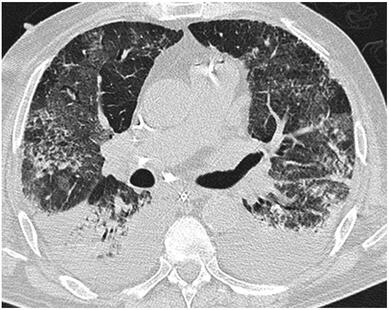
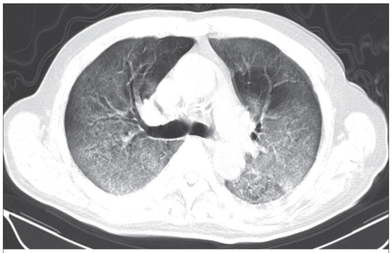
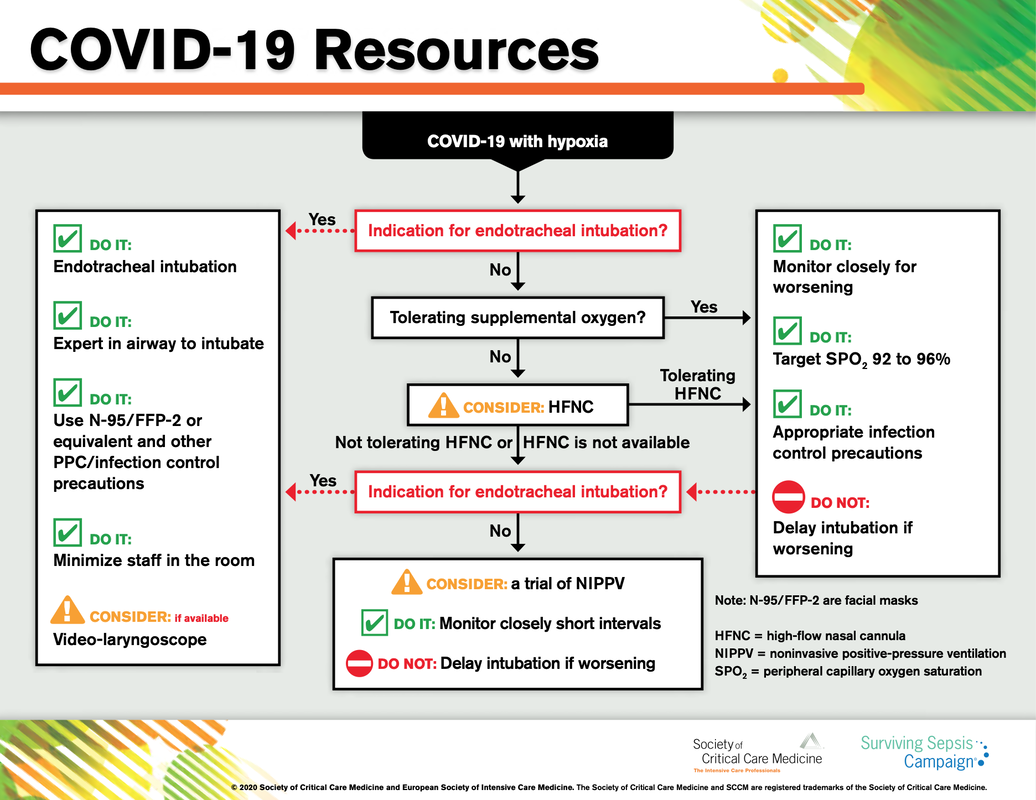
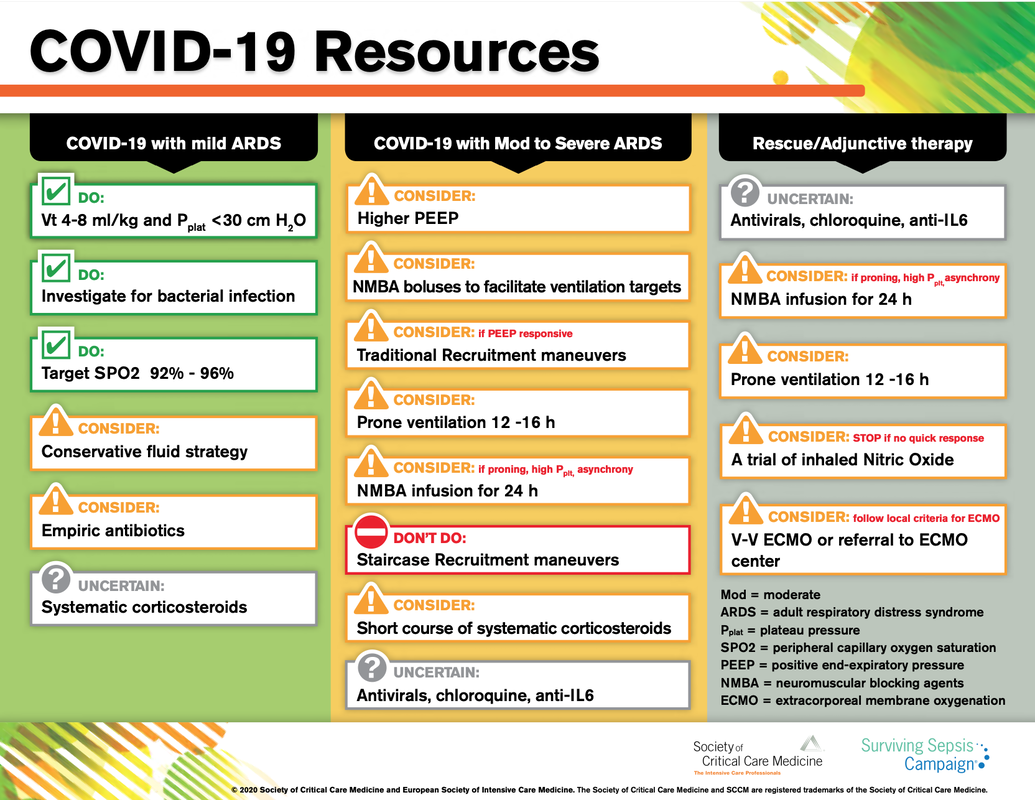
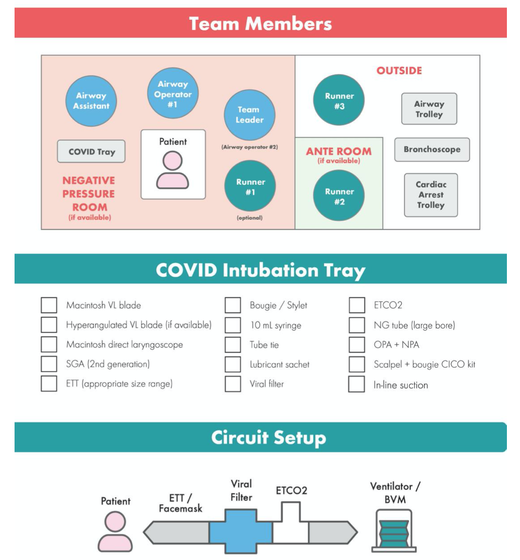
The lastest updated surviving sepsis guidelines for COVID-19 patient recommends a high-peep strategy in the intubated, mechanically ventilated patient. As most of these patients present with moderate to severe ARDS, PEEP is used to keep lung areas open and therefor to improve oxygenation. This seems to be especially true in the classical case of ARDS, where the lung become 'wet' and 'heavy' which results in widespread atelectasis of the dependent parts of the lungs, often further complicated by pleural effusions. Classical CT appearance in the acute phase of ARDS is an opacification with an antero-posterior density gradient. Dense consolidation in the most dependent regions merges into a background of widespread ground-glass attenuation and the normal or hyperexpanded lung in the non-dependent areas (Howling SJ et al. Clin Radiol 1998;53(2):105-109). The theory behind these changes is that the increased weight of overlying lung causes compression-atelectasis posteriorly. The fact that prone positioning these patients quickly redistributes these gradients supports this theory (Desai SR et al. Anaesthesiology 1991;74(1):15-23). Chest CT's in patients with COVID-19 often show ground-glass opacification with or without consolidations. These are changes often seen in viral pneumonia. Several case series suggest, that CT abnormalities seem to be mostly bilateral and tend to have a peripheral distribution, often involving the lower lobes. In contrast to the classical ARDS pleural thickening, pleural effusion and lymphadenopathy seem to be a less common finding (Shi H et al. Lancet Infect Dis 2020). The leading problem in COVID-19 patients with ARDS is hypoxemia, while hypercapnia does not seem to be a significant problem. Sometimes profound hypoxemia does not seem to correlate with patient symptoms at all. In regards to the images above, atelectasis might not be the predominant reason for V/Q mismatches in these patients. Observations of mechanically ventilated patients in our unit and other hospitals in Switzerland have shown, that higher PEEP levels (15cmH2O and higher) often result in significantly reduced compliance values complicating ventilation and favouring the development of pulmonary over-inflation. This observation might support the theory that patients with COVID do not represent the traditional manner of ARDS with distinctive atelectasis. Another observation that supports this theory is that COVID-19 patients often do not respond as clearly to Prone Positioning as classical ARDS patients do. More probably, V/Q mismatch seems so happen on a more microscopical level in COVID-Patients. Lung compliance is often normal on these patients and, therefore, applying high PEEP-levels does NOT add any benefit at all. Maybe the principle of less is more also applies to COVID-19 patients we treat (Gattinoni L et al. Intensive Care Medicine; 46, pages780–782(2020)) Looking at the New Surviving Sepsis Campain COVID-19 Guidelines: Given these considerations, the strategy with High PEEP-levels in general should be questioned in principle. The European Society of Intensive Care Medicine ESICM and the Society of Critical Care Medicine SCCM have been very efficient in providing us health care workers with a guideline manuscript giving recommendations on the treatment of COVID-19 patients in a critical care setting. It is imperative to keep in mind that research is moving forward very quickly in these times and changes to these recommendations are likely to occur. A collection of many reliable OPEN ACCESS platforms on SARS-CoV-2 can be found on www.foam.education. Infection ControlWhen performing aerosol-generating procedures on patients with COVID-19 in the ICU, fitted respirator masks (N95 respirators, FFP2) should be used (in combination with full Personal Protective Equipement PPE) Aerosol-generating procedures on ICU patients with COVID-19 should be performed in a negative pressure room During usual care for non-ventilated and non-aerosol-generating procedures on mechanically ventilated (closed circuit) patients surgical masks are adequate For endotracheal intubation video-guided laryngoscopy should be used, if available In intubated and mechanically ventilated patients, endotracheal aspirates should be used for diagnostic testing Supportive CareIn COVID-19 patients with shock, dynamic parameters like skin temperature, capillary refilling time, and/or serum lactate measurement should be used in order to assess fluid responsiveness For the acute resuscitation of adults with COVID-19, a conservative over a liberal fluid strategy is recommended For the acute resuscitation of adults cristalloids should be used - avoid colloids! Buffered/balanced crystalloids should be used over unbalanced crystalloids Do NOT use hydroxyethyl starches! Do NOT use gelatins! Do NOT use dextrans! Avoid the routine use of albumin for initial resuscitation! In shock use norepinephrine/ noradrenaline as the first-line vasoactive agent The use of dopamine is NOT recommended Add vasopressin, if target MAP cannot be reached Titrate vasoactive agents to target a MAP of 60-65 mmHg, rather than higher MAP targets For patients in shock and with evidence of cardiac dysfunction and persistent hypoperfusion despite fluid resuscitation and norepinephrine, adding dobutamine should be used For persistent shock despite all these measures, low-dose corticosteroids should be tried Ventilatory SupportKeep peripheral saturation SpO2 above 90% with supplemental oxygen
There is NO need for supplemental oxygen with SpO2 above 96% In acute hypoxemic respiratory failure despite conventional oxygen therapy, high-flow nasal cannulas (HFNC or High-Flow) should be used next High-Flow should be used over non-invasive ventilation (NIV) If High-Flow is not available and there is no urgent need for endotracheal intubation, NIV with close monitoring can be tried In the event of worsening respiratory status, early endotracheal intubation should be performed In mechanically ventilated patients, low-tidal volume ventilation should be used: 4 to 8 ml/kg In mechanically ventilated patients with ARDS targeting plateau pressures (Pplat) of < 30 cm H2O should be aimed for In patients with moderate to severe ARDS, a high-PEEP strategy should be used (PEEP >10cmH2O). Patients have to be monitored for potential barotrauma NOTE by Crit.Cloud: The strategy for high PEEP levels in general is currently discussed controversially. Observations in our own unit showed, that high PEEP levels tend to impaire compliance and therefor the quality of ventilation. Read also: "Less is More" in mechanical ventilatio, Gattinoni L. et al. Intensive Care Med (2020) 46:780-782 Patients with ARDS should receive a conservative/restrictive fluid strategy In moderate to severe ARDS, prone positioning for 12-16 hours is recommended To facilitate lung protective ventilation in moderate to severe ARDS, intermittent boluses of neuromuscular blocking agents (NMBA) should be used first In the event of persistent ventilator dyssynchrony, the need for ongoing deep sedation, prone ventilation, or persistently high plateau pressures, a continuous NMBA infusion for up to 48 hours should be used next Do NOT use inhaled nitric oxide in COVID-19 patients with ARDS routinely In severe ARDS and hypoxemia despite optimising ventilation and other rescue strategies, a trial of inhaled pulmonary vasodilator as a rescue therapy can be considered; if no rapid improvement in oxygenation is observed, the treatment should be tapered off If hypoxemia persists despite optimising ventilation, recruitment manoeuvres should be applied If recruitment manoeuvres are used, DO NOT use staircase (incremental PEEP) recruitment manoeuvres If all these measures fail, the patient should be considered for venovenous ECMO COVID-19 TherapyIn mechanically ventilated patients WITHOUT ARDS, systemic corticosteroids should NOT be used routinely In contrast, mechanically ventilated patients WITH ARDS, the use of systemic corticosteroids is recommended Mechanically ventilated patients with respiratory failure should be treated with empiric antimicrobials/antibacterial agents Critically ill patients with fever should be treated with paracetamol (acetominophen) for temperature control In critically ill patients standard intravenous immunoglobulins (IVIG) should NOT be used routinely Also, the routine use of convalescent plasma is NOT recommended The routine use of lopinavir/ritonavir (Kaletra®) is NOT recommended Currently, there is insufficient evidence to issue a recommendation on the use of other antiviral agents in critically ill adults with COVID-19 Currently, there is insufficient evidence to issue a recommendation on the use of recombinant interferons (rIFNs); chloroquine or hydroxychloroquine; tocilizumab (humanised immunoglobulin) The Aerosol-Danger of SARS-Cov-2The outbreak of the SARS Coronavirus-2 (SARS-CoV-2) in China 2019 has within a short time spread around the globe and is just about to hit central Europe. Although about 80% of all confirmed cases develop a mild febrile illness, around 17% develop severe Corona viral disease (COVID-19) with findings of acute respiratory distress syndrome (ARDS), of which about 4% will require mechanical ventilation. Since this virus, which was previously unknown to humans, spread rapidly around the globe, a large number of patients requiring intensive medical care now arise within a very short time. The lungs are the organs most affected by COVID-19 because the virus accesses host cells via the enzyme ACE2, which is most abundant in type II alveolar cells of the lungs. This results in mainly type 1 respiratory failure, which often requires urgent tracheal intubation and mechanical ventilation. Due to viral shedding in the patient's lungs, COVID-19 spread mainly via droplets. Events like coughing, high flow nasal oxygen (High-Flow), intubation and more can cause aerosol generation, allowing these airborne particles to travel even further distances. Performing endotracheal intubation in these patients is, therefore, a high-risk procedure, and it is required to adhere to certain principles to avoid infection of health care providers. The Safe Airway Societies of Australia and New Zealand have published a consensus statement that describes the problem very well and provides practical tips based on the currently available evidence. 1. Non Invasive Ventilation (NIV) and High Flow Nasal Oxygen (High-Flow)Current evidence suggests that the failure rate of NIV in COVID-19 patients seems to be similarly high as observed among Influenza A patients. Failure in these patients resulted in higher mortality. In general, NIV is recommended to be avoided or at least used very cautiously! The utility of High-Flow in viral pandemics in unknown. There is some evidence suggesting a decreased need for tracheal intubation compared to conventional oxygen therapy. High Flow Nasal Oxygen is worth a try, although it has to be assumed, that this is aerosol-generating. High-Flow should only be used in (negative pressure) airborne isolation rooms, and staff should wear full personal protective equipment (PPE) including N95/P2 masks. NIV and High-Flow are NOT recommended for patients with severe respiratory failure or when it seems clear that invasive ventilation is inevitable!
|
Search
|





 RSS Feed
RSS Feed


