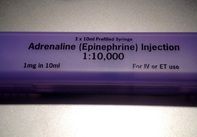
 Guidelines on advanced cardiopulmonary resuscitation around the world, including the ACLS guidelines, are based on four important concepts: mechanical resuscitation (CPR), defibrillation, airway management and also application of vasoactive drugs. The application of these drugs is intended to improve hemodynamics and the heart's responsiveness to defibrillation. What some of us might not be aware of though, but has already been mentioned by the '2010 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations' and the 'European Resuscitation Council Guidelines' in 2010: There is actually no definitive evidence that the application of these drugs provides any long-term benefit for these patients. While vasopressors are intended to improve coronary and cerebral perfusion and therefore successful defibrillation and neurological outcome, there is actually some concern (animal and registry studies) that this might actually decrease microcirculation and cerebral blood flow as well as increase myocardial oxygen consumption and cause post-defibrillation ventricular arrhythmias. Also the use of anti-arrhythmic drugs as well as their combination with vasopressors lacks evidence of any impact on survival. Another interesting fact is that we have no idea about ideal dosage or optimal timing of these drugs... should they be given continuously? This and many more questions and facts are discussed in an interesting review article by Sunde and Olasveengen in Current Opinion in Critical Care. They conclude that there is no evidence to support any specific drugs during cardiac arrest and that healthcare systems should not prioritise implementation of unproven drugs before good quality of care can be documented. Are we heading towards an era of drug-free resuscitation? Sunde K et al. Curr Opin Crit Care. 2014 April 16 Article accessible here Comments are closed.
|
Search
|


 RSS Feed
RSS Feed


