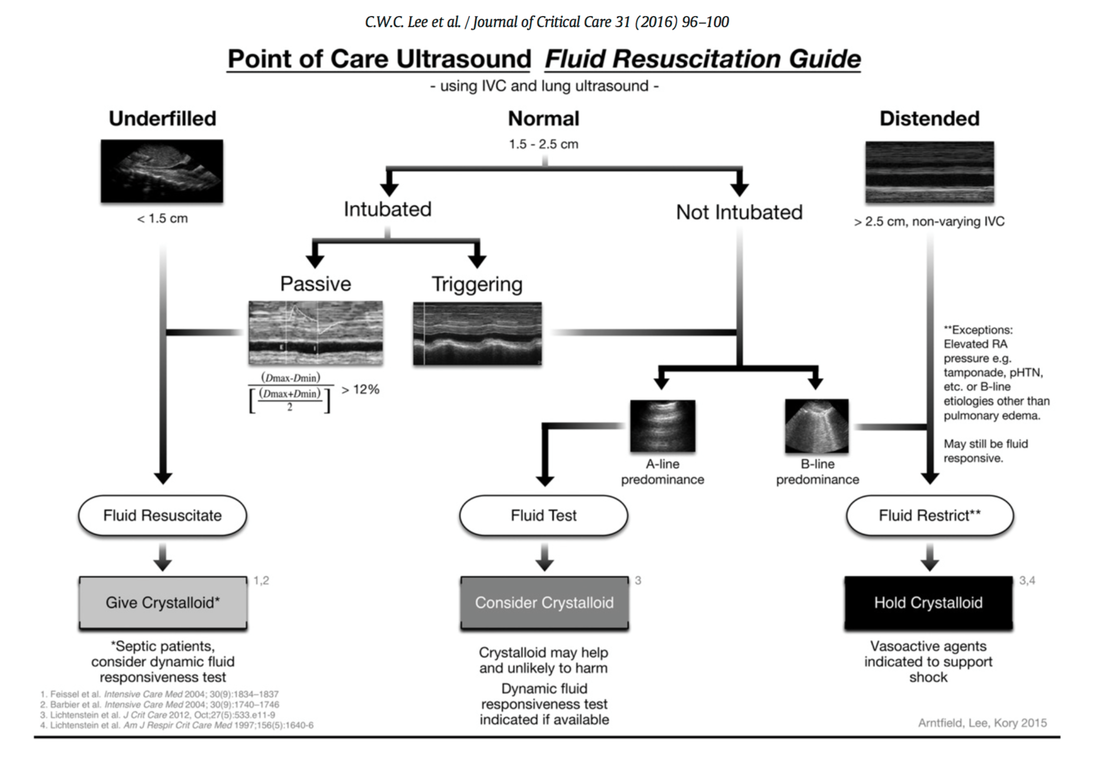
 Fluids are one of the cornerstones in the treatment of patients with shock. But with any drug applied, also fluids can harm if given inappropriately! While inadequate fluid resuscitation might result in tissue hypoperfusion and worsening of end-organ function, to much fluid might lead to problems like pulmonary oedema and finally increased mortality. Many measures are used in clinical practice, but most of them lack specificity and are not very representative as a sole marker. One of the better methods to evaluate fluid requirements is the use of dynamic measures that estimate the change in cardiac output (CO) in response to a fluid bolus. In this regard the use of point-of-care ultrasound (POCUS) has become increasingly attractive in order to use basic critical care ultrasound to asses the need of fluids in a specific clinical setting. Lee at al. have now looked at the sonographic assessment of the inferior vena cava and lung ultrasound in order to quite fluid therapy in intensive care. By taking into account current evidence they have produced an algorithm using these measures to help guiding fluid therapy. As with any measurement in critically ill patients the pathophysiologic cause of shock must be taken into account. The algorithm presented here seems to work best in patients in hypovolemic shock. To fully understand the following algorithm and its limitations we recommend to read the open access article (see link below). In conclusion: The algorithm provided is a helpful tool to help assess the need of fluids in a simple and quick manner. Lee C et al. J of Crit Care 31 (2016) 96-100 OPEN ACCESS Comments are closed.
|
Search
|


 RSS Feed
RSS Feed


