|
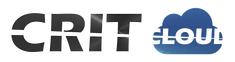
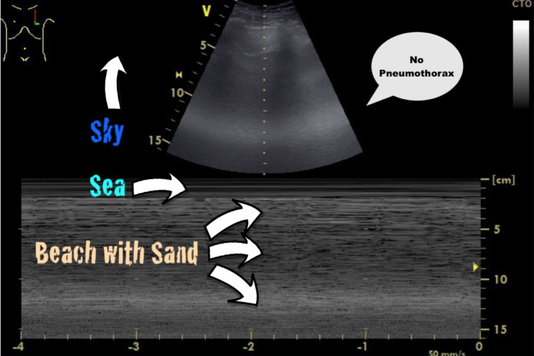
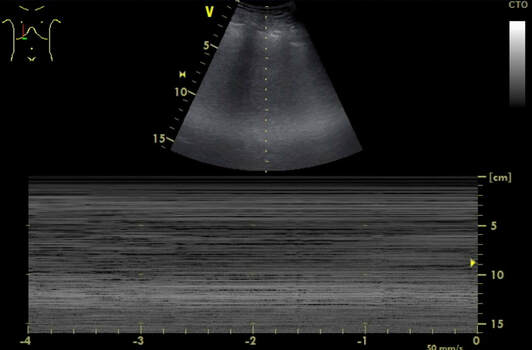
Central venous lines a commonly used in critical care and normally don't cause too many problems. They are though associated with potentially severe complications like infection, thrombosis, occlusion, bleed and of course pneumothorax on insertion. Although the usage of ultrasound guidance minimises the risk of the latter, there remains a restriction risk of this happening, giving you the challenge to solve this problem professionally. The CaseA 67-year old lady needed the insertion of a central venous catheter during surgery, which the anaesthetist performed with the aid of ultrasound but of course under aggravated conditions. When brought into the critical care unit postoperatively she presented with no audible breathing sound on the right side of her chest. An ultrasound (US) of the right lung showed no visible pleural gliding, and in M-mode only 'sea' but no 'beach' or 'sand'. To estimate the extent of the pneumothorax, we performed a pa chest x-ray (CR), which confirmed the diagnosis. The image showed an apical interpleural distance of 3cm and laterally of 2-3cm. How often does this happen? Could I have prevented this complication? What would you do in this situation? To answer these and some other questions we performed a quick review of current literature and provide a short review. Are iatrogenic pneumothoraces common?It's a fact: Iatrogenic injuries are an inevitable part of medicine. Emergent procedures performed in the emergency department (ED) present a higher risk for iatrogenic injury than in more controlled settings (Swain et al., 2005; Mort, 2004). This fact implies that you should NEVER perform a procedure if you cannot handle the potential complications. A procedural error followed by mismanagement increases the likelihood of morbidity and mortality immensely. The incidence in the literature varies from 0 to 6% (numbers are higher in emergencies), bearing in mind, that depending on the control method used (US, CR or none), some are just not diagnosed. Subclavian vein insertion has been reported to have a higher incidence of pneumothorax than internal jugular vein insertion. What can I do to prevent iatrogenic pneumothoraces?- Make sure that there is an indication for central venous access (e.g. vasopressors in low to moderate doses are no absolute indication, PulmCC: Are central lines really needed for vasopressor infusions?) - Use a standardized method of CVC insertion in your unit or institution - Insertion by experienced physician (performing more than 50 CVC insertion a year) or at least his assistance has proved to lower the risk of pneumothorax - The use of ultrasound during CVC catheterization reduces the time required for insertion and the rate of mechanical complications How do I diagnose a pneumothoraxIatrogenic pneumothorax might not cause any clinical symptoms, especially in the young and otherwise healthy patient. Symptoms might include chest pain (sometimes radiating to the ipsilateral shoulder), shortness of breath (to life-threatening respiratory distress) and less commonly cough, anxiety or malaise. On examination, you might find tachypnoea, asymmetrical lung expansion, unilaterally decreased breath sounds. Cardiovascular findings might include tachycardia, hypotension, pulsus paradoxus and jugular venous distension (often present in tension pneumothorax). Subcutaneous emphysema and tracheal deviation might occur occasionally. A definite diagnosis is made by performing chest radiography (CR), CT-scan or bedside ultrasonography (US). Supine chest radiographs are unreliable in making the diagnosis of pneumothorax, with a sensitivity value of 36%. US is more sensitive than supine CR and as sensitive as CT in the detection of pneumothoraces. Performance of US for the detection of pneumothorax is excellent and is superior to supine CR. Considering the ease of access and the outstanding clinical performance of US (numerous studies have described near 100% sensitivity and 90% to 95% specificity if a thorough examination is performed), current studies support the routine use of US for the detection of pneumothorax. - Clinical signs are unspecific and might not be present - Ultrasonography is the first choice for the detection of pneumothorax - For a general evaluation of the size of a pneumothorax, an erect chest x-ray in inspiration is recommended - CT scans are only recommended for uncertain or complex cases Does every central line need a chest x-ray after insertion?CR of supine patients is not sensitive enough to identify hidden pneumothorax because the air initially dissipates within the nondependent and medial parts of the chest and therefore can be invisible on supine radiographs. Even upright CR can be challenging and unreliable. Also, CR is often performed immediately after CVC insertion and it is therefore possible that there is not enough time for the development of a pneumothorax large enough to be identified. - Routine CR after central line insertion is unreliable and not necessary: It's an inefficient screening tool! - Current evidence supports the use of US to exclude iatrogenic pneumothorax How do I treat an iatrogenic pneumothorax?If a pneumothorax occurs during the insertion of a central line urgent action might not be necessary. If asymptomatic, you might proceed with the central line insertion when the patient is in urgent need. - If signs of a tension pneumothorax arise, a simple needle decompression or urgent chest drain is life-saving and allows for a continued controlled attempt of the central line on the same side (you can’t cause a pneumothorax twice). - Never attempt a central line insertion on the opposite side to avoid bilateral iatrogenic complications! - In the setting of iatrogenic pneumothorax the BTS guidelines on the management of spontaneous pneumothorax can be applied: - Remember: If the inter-pleural space on CR is less than 2cm (some allow 3cm as an upper limit) and the patient remains asymptomatic, conservative treatment is appropriate! - Apply nasal oxygen 3-5L/min (see below) - A follow up chest x-rax after 12-24 hours is advisable. Did you know? When no supplemental oxygen is applied air is reabsorbed spontaneously by 1.25% of pneumothorax size per day. Oxygen administration at 3 L/min nasal canula or higher flow treats possible hypoxemia and is associated with a fourfold increase in the rate of pleural air absorption compared with room air alone. Got interested? Get more info here: |
Search
|


 RSS Feed
RSS Feed


